Online shopping provides a quick and convenient way to purchase products, and this is especially true for the...
DVT Pumps | DVT Compression - DVT Therapy - DVT Pump Comparison
DVT Pumps are pneumatic compression pumps designed to prevent people from getting deep vein thrombosis (DVT), which can be life-threatening. DVT Compression Pumps deliver pressure to increase blood flow in the venous system of the limbs so that blood does not clot. Those who are especially susceptible to thrombosis are people who recently had surgery or who are immobile or sedentary throughout the day. Prolonged inactive states often cause blood
What is DVT?
Deep vein thrombosis is a blood clot that forms in a vein deep inside the limbs of the body. It "is the formation of a thrombus in the deep venous system that if untreated, can lead to non-fatal or fatal pulmonary embolism (PE). In 1998, the Journal of American Medical Association reported approximately 2 million Americans each year suffer from DVT, and it is considered the 3rd most common cardiovascular disease after acute coronary disease and stroke."1 "Deep vein thrombosis (DVT) is a major health problem, which affects 1 in 1000 people in the general population each year. It may be asymptomatic or cause swelling and pain, and can lead to potentially fatal complications."2 In most cases, this clot forms inside one of the deep veins of the thigh or lower leg.
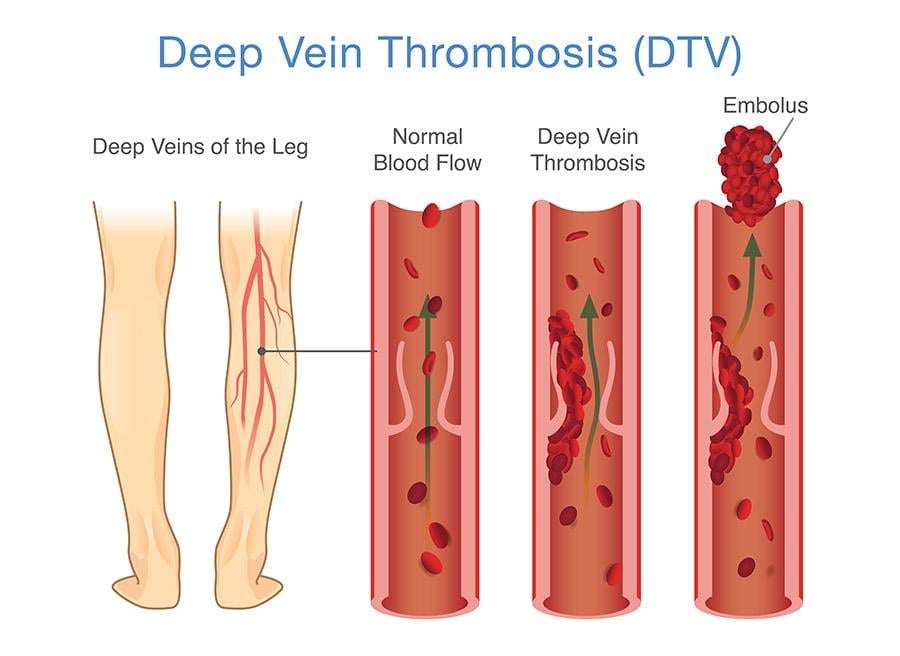
Veins are the blood vessels that bring oxygen-depleted blood and waste back to the heart. The veins in your legs have tiny valves that help keep blood moving back up towards the heart. But a DVT may damage one or more of these valves. This damage causes the valves to weaken or become leaky. When this happens, blood starts to pool in the legs. DVT can also occur if people are immobile for an extended period. The movement of the leg muscles helps blood traverse up the veins as the muscles contract. When blood flows very slowly through the veins from being sedentary, there is an increased risk that cells in the blood will stick together and form a dangerous clot.3
The application of mechanical pneumatic compression promotes blood circulation and increases systemic fibrinolytic action for the prevention of venous thromboembolism. Improved blood circulation helps with thrombosis prevention. Pneumatic compression has few side effects, stands as an important alternative to chemical prophylaxis, and supports patients with a high risk of bleeding.4 This leg pump compression also inhibits blood platelet aggregation, one of the leading causes of DVT.5
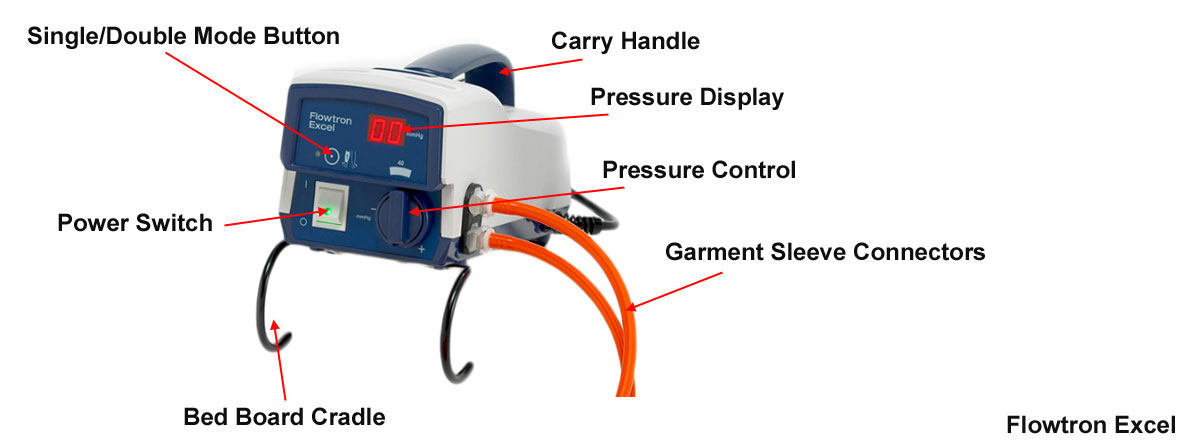
Anatomy of a DVT Compression Device for Deep Vein Thrombosis Prevention
Advantages of Deep Vein Thrombosis Prophylaxis Device
- Accelerates blood flow
- Reduces capillary filtration
- Increases blood flow
- Increases partial oxygen tension in the skin
- Normalizes endothelial adhesion of leukocytes
- Tightens intracellular junctions
- Restores structural changes in media myocytes in stripped veins
- Treats chronic venous disease
- Treats venous ulceration
- Treats varicose veins
- Treats post-thrombotic syndrome
- Prevents DVT or blood clots
- Painless unless some other underlying cause
- Prevents venous stasis
- No side effects common to blood-thinning medications
Disadvantages of DVT Leg Pump
- Requires correct application by caregiver or patient
- Patient compliance issues
- Knee or leg surgery restricts the size or length of the sleeve and a foot sleeve may be used in these instances.
- Some experience discomfort
- Some experience skin breakdown
- Some experience nerve damage (rare)
- Some experience pressure injuries (rare)
- Sweating underneath the compression sleeve
- Excessive warmth underneath the sleeve
How to Select the Best DVT Pumps FOR SALE
Deep Vein Thrombosis Pump Continuum
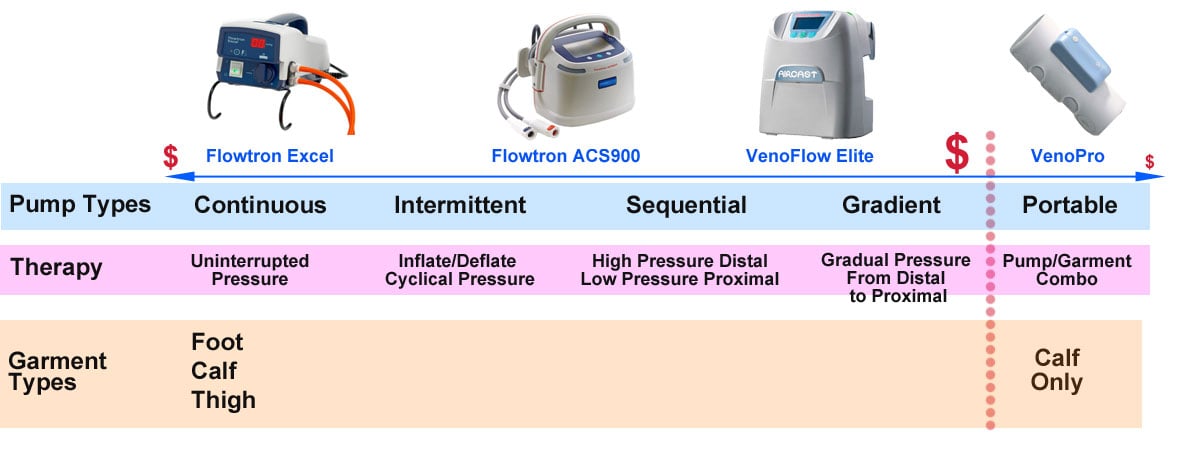
Always start with the doctor's recommended pump type. For chronic conditions, the bedside leg compression pumps displayed on the continuum just right of center and going left to the beginning of the continuum are a necessity. The products on the far left of the continuum (continuous DVT pressure pumps) offer limited functionality but serve the majority of patients well. As you move towards the right of the continuum, product functionality increases with intermittent, sequential, and gradient treatment options. These advanced options also increase the purchase price. Most often, these devices are sold with the pump separate from the garment, allowing you to select your garment size. The ultimate devices offer a combination of sequential and gradient therapies. The far-right portable products are lightweight, tubeless, easy to don and doff and have the lowest purchase price. However, portable DVT pumps also have the shortest product lifespan.
Types of DVT Compression Therapy Pumps
Continuous Compression provides uninterrupted pressure to the garment or sleeve. This compression therapy noninvasively reduces the incidence of deep vein thrombosis (DVT), pulmonary embolism (PE), and Venous Thromboembolism (VTE), all potentially life-threatening conditions. Most often, continuous therapy occurs through the use of compression stockings.
Sequential Compression Devices (SCD) employ a compression pump and arm, leg, or foot sleeves with multiple air bladders that wrap around the limb and inflate with air one at a time. This sequential inflation in which the lower air pockets inflate first, then the middle pockets inflate second, and the upper inflate last, imitates walking and helps prevent blood clots. Patients at risk for DVT should undergo compression therapy under the advice of a physician while in bed or sitting in a chair.6
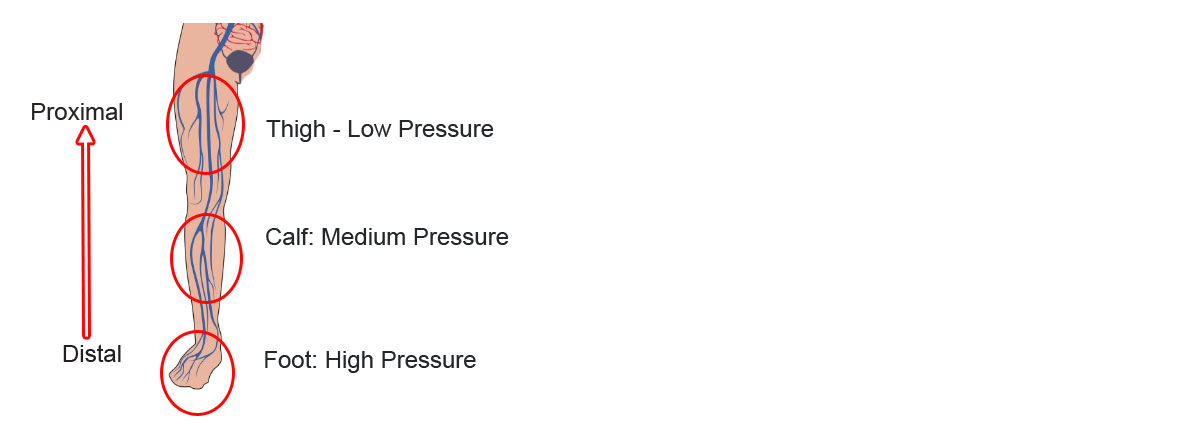
Gradient Compression Devices (GCD) use gradual compression to force venous blood back into circulation. It applies pressure on the lower extremities like the foot, ankle, calf, and upper leg to stimulate blood flow and prevent blood from clotting. With gradient compression, the pressure is higher on the distal end of the leg and gradually decreases the further you go up the proximal part of the leg. This high distal to low proximal pressure helps increase the flow of blood upward toward the body. Gradient compression takes place with special Deep Vein Thrombosis Compression Stockings or with DVT Pump Sleeves.7
Intermittent Compression inflates cuffs and then slowly deflates and relaxes. The cycle of inflating and deflating occurs over and over to help move blood up through the veins. It also promotes the natural release of substances into your bloodstream that helps to prevent clots. During the relaxing part of the cycle, oxygen and nutrient-rich blood continue to flow through the limb under treatment. DVT intermittent compression is a useful tool to prevent DVT, PE, and VTE.
Cryocompression or Continuous Flow Cryocompression (CDC) is a combination of compression therapy and cold therapy. It utilizes a compression sleeve that also has continuous flowing ice-cold water to prevent and reduce swelling. Cold water also provides a mild analgesic effect. (Leegwater) Often used for hip and knee post-op surgery, this therapy represses swelling and reduces the risk of forming blood clots.

Continuous Sequential compression therapy provides uniform and sequential compression. This therapy involves a single cuff to deliver uniform and sequential therapy from a single pump.
Gradient Sequential leg compression increases blood flow and encourages extracellular fluid clearance. These graduated compression devices provide cycles of compressed air at adjustable pressures. The pump inflates and deflates garments to move fluid up the leg. The pressure at the distal end of the leg is higher than the pressure at the proximal end. Pressure inflates sequentially at the distal end and gradually moves up toward the proximal end of the leg until all segments complete inflation. Then all segments deflate at the same time.
"Graduated or graded sequential compression uses multiple bladders to compress the limb in a "milking" action. The cuffs are sequential because the most distal bladder inflates first and the most proximal bladder last and are graded because the most distal bladder will inflate to the highest pressure and the most proximal to the lowest."8
Non-segmented or single-chambered compression sleeves only have a single chamber garment that inflates and deflates.
Segmented or multi-chambered compression garments provide for air chambers to inflate and deflate in a sequence to push blood and fluids up the limb. Multi-chambered sleeves and their corresponding pumps offer more advantages than a single-chambered version.
Calibrated Compression Therapy Pumps deliver individually determined pressure to each garment segment. Segments usually range between three and eight. The length and frequency of the inflation cycles are also adjustable, allowing the most control over the therapy administered to the patient. These systems allow for manual control of the location and the intensity of the compression to meet the patient's tolerance and the patient's circumstances for the specific area affected. The ability to program the pressure in each segment with a calibrated gradient pressure more closely mimics the natural action of the body's circulatory system. Some DVT devices customize compression cycles automatically for each patient, like the Kendall SCD 700 Smart Compression Controller.
Circumferential Compression offers positionally independent compression on all sides of the leg. Circumferential pressure helps to reduce the risk of VTE through the use of specially designed DVT Sleeves or mechanical compression garments.
Passive Compression consists of knee and thigh-high Compression Stockings or Arm Sleeves. Elastic stockings provide continuous pressure and often uniform pressure (the same pressure throughout the stockings' length) or graduated compression (higher pressure at the distal end and lower pressure at the proximal end). Anti-Embolism Stockings are also available to help control venous and lymphatic pooling. Stocking therapy helps reduce the incidence of DVT and stands as the first tier for compression therapy.
Active Compression involves external pneumatic compression using a DVT compression pump with leg or arm garments. These venous foot pumps and leg pumps offer a second tier of compression therapy for DVT prevention.
Non-calibrated Compression pumps typically involve a single pressure control on the distal segment. The pump then applies the same sustained pressure in each subsequent segment as they inflate going up the leg.
Programmable Pumps provide for control over the amount of pressure to each garment segment and the interval span. This feature allows caregivers or patients to set a comfortable therapy session that best meets individual needs and increases patient compliance.
Non-programmable and non-adjustable pumps offer sustained pressure that is not adjustable. These types of pumps have more problems with patient compliance, particularly when the patient does not tolerate well the sustained pressure.
Sequential Compression Devices (SCD) utilize sleeves that have multiple pockets that inflate with air pumped from the intermittent pneumatic compression pump. The air pocket farthest from the heart balloons first, and then the next farthest air chamber expands in a sequential circulator fashion forcing blood up the limb. Each air cavity fills and exerts pressure in a sequence that causes trapped blood to flow up the leg. This sequence improves venous circulation in the limbs of patients at risk of DVT or PE. Sequential DVT pumps are very popular.
Portable DVT Machines
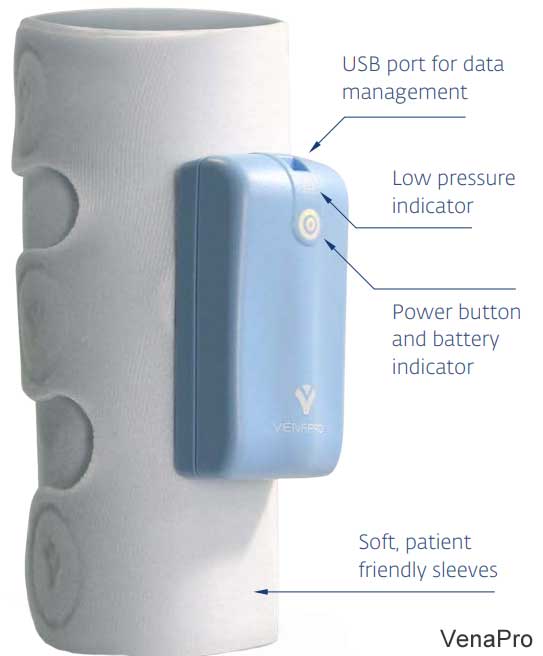
Portable DVT Devices allow therapy in the home, hospital, workplace, and while traveling. These DVT prevention devices stimulate blood circulation in the legs to prevent blood clots. The pump is built-in in the garment that wraps around the leg and secures with hook-and-loop closure. The garments mimic the body's natural muscle contractions to increase venous blood flow. The best-selling models include the Bio Compression IC1200 Vascu-Ease, DJO VenaPro, the Devon Cirona 6300, and Cirona 6400. Each of these portable sequential compression devices is easy to use and provides quick application. The portable pump/garment combo is less expensive than the other options but also has a short product life.
It is important to note that there are also Lymphedema Compression Pumps for Legs. Lymphedema pumps should not be used to treat deep vein thrombosis. In fact, the presence of DVT is a contraindication for the use of a lymphedema pneumatic device.
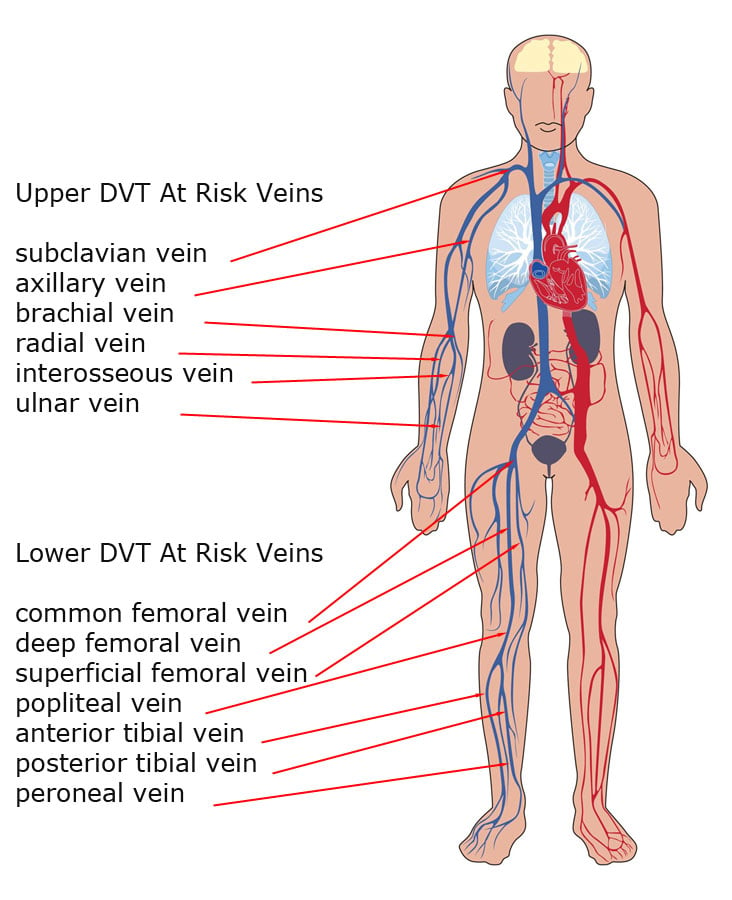
Deep Vein Thrombosis Anatomy
- Paired radial vein
- Paired ulnar vein
- Interosseous vein
- Brachial vein
- Axillary vein
- Subclavian vein
- Common femoral vein
- Deep femoral vein
- Superficial femoral vein
- Popliteal vein
- Anterior tibial vein
- Posterior tibial vein
- Peroneal vein9
DVT Pump Indications
- Immobile patients
- Patients with a history of DVT/PE
- Critical ill patients admitted to intensive care unit (ICU)
- Stroke with lower extremity paralysis
- Advanced congestive heart failure (CHF)
- Active cancer
- Acute respiratory failure
- Thrombophilia
- Recent surgery or trauma
- Obesity
- Ongoing hormonal therapy10
Deep Vein Prophylaxis (Mechanical) Contraindications
- Limb ischemia due to peripheral vascular disease
- Skin breakdown11
DVT Complications
Failure to prevent DVT in hospitalized patients increases the risk of forming blood clots. Complications of DVT include the following:
- Pulmonary Embolism - This occurs in one-third of patients with DVT. Pulmonary embolism can be life-threatening. Even when treated, patients may develop pulmonary hypertension.
- Post-thrombotic Syndrome - Symptoms PTS include limb swelling, pain, discoloration, itching, and ulcer formation.12
Mechanical Prophylaxis Treatments
- Intermittent pneumatic compressions (IPC)
- Graduated compression stockings (GCS)
- Venous foot pump.13
FAQ's
What is a DVT machine?
A Deep Vein Thrombosis Pump is a pneumatic compression device that non-invasively increases blood circulation in the limbs of the body. Cuffs wrap the arms, legs, or foot and attach to a pump that provides pressure to the limb. This pressure improves blood flow to decrease the risk of forming blood clots.
How does compression prevent blood clots?
Compression to the arms or legs helps keep blood from pooling in the limbs of the body. Mechanical compression helps to improve venous circulation and reduce the risk of blood clots. Inflatable auxiliary sleeves, gloves, or boots stimulate blood circulation to decrease the risk of pulmonary embolism and deep vein thrombosis. The inflatable pressure forces blood out of the limbs and back into the torso.
How does a DVT pump work?
An immobile patient "may have pneumatic compression boots prescribed to prevent deep vein thrombosis (DVT). Attached to a pump and applied to one or both legs, the boots are fabric wraps containing bladders that inflate intermittently to compress the legs and propel the blood forward. Styles are available for use on the calves only or the thighs and calves…. Intermittent compression pushes blood from the smaller blood vessels into the deeper vessels and up to the femoral veins. The accelerated blood flow decreases venous stasis and congestion, flushes out locally activated clotting factors, and promotes fibrinolysis. The compression decreases vessel distension, which lowers the risk of injury to the endothelial layer."14
How do you prevent DVT?
- If you are overweight, lose weight.
- Stay active throughout the day.
- Go on walks twice daily.
- Avoid long periods of being still and inactive.
- Exercise regularly.
- Ask your doctor about blood thinners or compression stockings to prevent blood clots.
After surgery, what are those wraps they put on your legs?
DVT Pumps or intermittent pneumatic compression (IPC) devices help prevent blood clots in the deep veins of the legs. These devices use sleeves with pockets around the legs that fill with air and apply pressure to your legs. This pressure increases blood flow through the veins of your legs and helps prevent blood clots.

Does moving your legs while sitting help prevent blood clots?
Yes, any movement is helpful. Walking is very beneficial. On long trips, move your legs frequently and exercise your calf muscles to improve blood flow. Compression stockings may also help to minimize the risk of developing complications.
What should you not eat with DVT?
- Avoid excessive carbohydrates and processed foods.
- Reduce unhealthy fats and sodium.
- Eat low-fat, high protein foods.
- Eat plenty of fruits and vegetables.
- Eat whole grains bread and cereals.
Does compression therapy really work?
Yes, mechanical compression therapy does work. It is effective in preventing and treating DVT. "Thromboprophylaxis for at-risk inpatients can reduce VTE by 30 to 65 percent, has a low incidence of major bleeding complications, and has well-documented cost-effectiveness."15
What are the dangers of blood clots in the legs?
Blood clots can pose a serious danger if not treated. "[A]s many as 900,000 people could be affected (1 to 2 per 1,000) each year in the United States. Estimates suggest that 60,000-100,000 Americans die of DVT/PE (also called venous thromboembolism)."
- 10 to 30% of people will die within one month of diagnosis.
- Sudden death is the first symptom in about one-quarter (25%) of people who have a PE.
- Among people who have had a DVT, one third to one half will have long-term complications (post-thrombotic syndrome) such as swelling, pain, discoloration, and scaling in the affected limb.
- One-third (about 33%) of people with DVT/PE will have a recurrence within 10 years.
- Approximately 5 to 8% of the U.S. population has one of several genetic risk factors, also known as inherited thrombophilias in which a genetic defect can be identified that increases the risk for thrombosis...."16
What are the symptoms of DVT or blood clots in the leg?
- Discoloration in the leg or arm.
- Swelling.
- Pain.
- Warmth.
- Tenderness.
Can blood clot in leg kill you?
Deep Vein Thrombosis—The Blood Clot That Can Kill. According to the National Blood Clot Alliance, 274 people will die every day from the consequences of a blood clot. ... A deep vein thrombosis (DVT) occurs in the deeper veins-for example in the lower leg or calf
Are you hospitalized for blood clots in the leg?
Often, the recovery period associated with surgery and hospitalization and its sedentary positioning for an extended time increases the risk for blood clots. DVT prevention is a significant concern for most hospitals. Compression therapy through DVT pumps and stockings is commonplace in-hospital recovery programs.
Is DVT completely curable?
After treatments from your doctor, DVT is not likely to return if you exercise and walk daily. Avoid long periods of sedentary postures. Being active is the best long-term medicine.
Can sleep in a chair cause blood clots?
Any extended sedentary periods place people into a higher risk of DVT. Activity, exercise, and walking can do much to help you feel better and stay better. Muscle movement from walking or exercise compresses the veins to improve your circulatory system with proper blood flow. Long periods of sitting decrease your blood circulation.
How often should you do compression therapy?
For many patients, 20 to 30 minutes of compression therapy supplemented by the use of compression stockings is all that is required. However, each patient is different. It is essential to follow the instructions from your doctor to improve your circulatory health.
How much does compression therapy cost?
Ten weeks of outpatient treatment with compression therapy equipment ranges from $1500 to $3600. DVT treatment with compression pumps and sleeves offers reliable and cost-effective healing for most patients.
Does exercise help deep vein thrombosis (DVT)?
Yes, exercise does help to prevent and treat DVT. Walking is safe in acute deep venous thrombosis and can often improve severe symptoms. Exercise stimulates blood flow and strengthens the muscles around your blood vessels.
For patients who are unable to be active, compression therapy is essential. "Sequential intermittent compression with high pressures, 10 compression cycles three times daily, is recommended for all patients unable to undertake physically active prophylactic measures. An absolute indication exists in those patients who cannot be mobilized and those in whom there are additional contraindications to the use of anticoagulants. Sequential compression is no alternative to antithrombosis stockings which must be worn from the day of hospitalization until discharge and also during the period of pneumatic compression."17
Does a blood clot feel like a pulled muscle?
A blood clot feels very similar to a leg cramp, pulled muscle, or "Charley horse." Additionally, your leg may be swollen and sensitive to touch. Many DVT patients complain of their leg feeling extra warm and somewhat discolored. These symptoms of a blood clot may feel similar to a pulled muscle or a "Charley horse." There may be swelling, slight discoloration, and warm sensation in the leg or arm. These symptoms or warning signs are severe and merit calling your doctor as soon as possible to schedule an exam, because you may need treatment immediately.
How do you treat a blood clot in the leg at home?
First, see a doctor for a professional diagnosis. Your doctor may prescribe compression stockings that offer gradient compression that is higher at your foot and decreases as you go up the leg. These stockings improve blood circulation to keep blood from pooling and clotting. You may also benefit from a DVT compression pump with leg sleeves that provide adjustable pressure to prevent DVT from forming.
Elevating your legs while you are at home is very helpful. Take daily walks that offer your legs exercise. Standing on your tip-toes for a minute or two several times each day helps to constrict the blood vessels. This constriction promotes blood circulation.
Does a blood clot in the leg hurt constantly?
Blood clots often cause swelling, tenderness, and pain. Tightness in the affected limb, along with persistent and throbbing cramp-like symptoms, accompany blood clots. Walking may be difficult and painful. These symptoms may indicate that you have deep vein thrombosis.
Where in the leg do blood clots form?
The lower leg is the most common location for a blood clot to form. Blood returning to the heart has a more difficult time traversing against gravity. The valves in the veins may not function as needed creating a higher risk of clotting. Clots cause swelling and pain. A blood clot that breaks loose and travels to the lungs is a severe condition that often leads to morbidity. Blood clots can also form in the arms but are less likely. See the DVT Anatomy Graphic for more details.
How long does it take for a DVT to form after surgery?
After surgery, the critical period is between 2 to 10 days. Orthopedic surgery to the hips or knees highly increases your risk of developing DVT. Ortho patients continue to remain at risk after surgery for about 3-months. Your doctor may prescribe chemical or mechanical prophylaxis. Chemical treatments are invasive, but mechanical are external and non-invasive. Mechanical therapies may consist of compression stockings or a pneumatic compression pump with sleeves.
Can I fly with a DVT in my leg?
An airline passenger that has a previous diagnosis of DVT should consult with their physician before conducting any extensive travel. Anyone who has had DVT in the past is at increased risk of developing them again while flying. Anyone recently treated for DVT should wait for at least 4-weeks before traveling. Ask your doctor if you can safely travel and what measures you can take to prevent DVT while on your journey.
If you've received a diagnosis of DVT in the past or have a family history of blood clots, you're at an increased risk for developing them while flying. ... Some experts recommend waiting to fly on an airplane for at least four weeks after having DVT or PE, but talk to your doctor about this.
What does compression therapy do?
Compression therapy is a non-invasive and effective means of increasing blood flow to prevent DVT. The compression usually takes place on the lower limbs to force blood circulation. Applying pressure to the foot, ankles, and legs takes place through the use of compression sleeves with pressure supplied by a DVT compression machine. DVT stockings with pump include compression garments and a pneumatic pump that provides pressure to the DVT garments.
Does DVT hurt to touch?
Yes, DVT usually involves pain, swelling, skin sensitivity to the touch along the course of the vein. Often a bluish discoloration accompanies DVT near the clot area where blood is trapped.
How do they check for blood clots?
Ultrasound is the go-to device for diagnosing DVT or blood clots in the leg or arm veins. Ultrasound is a non-invasive test. Sometimes venography testing with dye, which is invasive, is necessary to provide more accurate results. Sometimes the more costly process of an MRI (magnetic resonance imaging) is necessary.
What are the risk factors for DVT?
You need to consider many different factors in assessing a patient's degree of risk for DVT. While there are no clear-cut distinctions between low, medium, and high risk, the general rule is "more is worse"—that is, the more of the following risk factors your patient has, the higher the risk of developing DVT:
- Age over 20
- History of venous problems
- Obesity
- Immobilization
- Lengthy surgical procedure
- Malignancy
- Congestive heart failure
- Cardiac arrhythmias
- Surgery in which thromboembolism is a common complication….
Of these risk factors, the most significant are the first two—age over 40 and a history of venous problems. Many of your patients probably have at least some of these risk factors. Deep vein thrombosis and its sequelae—chronic venous insufficiency and pulmonary embolism—are widespread. In fact, each year in the United States, two million cases of DVT, 800,000 cases of chronic venous insufficiency, and 600,000 cases of pulmonary embolism are diagnosed…. [M]any of these patients will benefit from the use of graduated compression stockings or a pneumatic compression device.18
What is the best treatment for DVT?
Without prophylaxis up to 70% of patients having major hip surgery will have a DVT. There is ample evidence that low-dose heparin can reduce this incidence, but with an increased risk of major bleeding. This also applies to the newer low-molecular-weight heparins (Drug and Therapeutics Bulletin 1993). Interest in mechanical methods of prophylaxis is increasing, since they may be as effective as heparin but with fewer disadvantages. Elastic compression stockings reduce the diameter of vessels and increase the velocity of returning venous blood. Electrical stimulation of leg muscles also increases return velocity but is painful and not well tolerated after operation (Browse and Negus 1970). There are a number of systems which provide intermittent pneumatic compression. These help to empty veins and also to release endothelial factors which stimulate fibrinolysis, but they do not reproduce the physiological mechanisms of venous return (Cam, Miranda and Greene 1986). The discovery of a physiological pump in the foot which is activated by flattening the plantar arch has led to the development of an apparatus which can provide intermittent plantar compression. This mimics the haemodynamic effects of walking and has been shown to eject venous blood towards the heart with sufficient force to overcome a cuff around the calf inflated to a pressure of 100 mmHg (Gardner and Fox 1993). These originators have used fluoroscopic phlebography to show that such intermittent compression of the venous foot pump creates turbulent flow in valve pockets, at the most common location for thrombus formation. They have also shown that use of the device induces a hyperaemic state with a reduction in peripheral resistance and an increase in arterial flow (Gardner and Fox 1993).
Other recent studies have shown that shear forces on venous endothelial cells cause the release of endothelial-derived relaxing factor (EDRF). This diffuses into arteriolar afferents, relaxing their musculature and thereby augmenting blood flow (Griffith and Randall 1989; Falcone and Bohlen 1990; Morgan et al 1991). EDRF inhibits platelet aggregation and probably stimulates disaggregation (Griffith and Henderson 1989). The use of an intermittent impulse device has also been shown to reduce postoperative oedema and pain. Oedema may itself cause a reduction in arterial flow and venous emptying, while venous congestion lowers pH, which contributes to the development of pain (Gardner et al 1990). The removal of accumulated fluid from the calf also lowers compartment pressures and reduces the risk of compartment syndromes.19
Do clinical studies support DVT treatment by compression pumps?
Yes, there are numerous studies that find a significant reduction in DVT incidence by the use of these prophylaxis devices. One study found the "[s]equential intermittent leg compression clinically and statistically significantly reduced the frequency of both proximal vein and calf vein thrombosis."20 Another study found "Intermittent pneumatic compression as used in this trial is a safe, effective, and extremely practical method of preventing postoperative deep vein thrombosis in patients not suffering from malignant disease."21 A treatment comparative study found that "IPC devices decreased the relative risk of DVT by 62 per cent when compared with placebo, 47 per cent compared with graduated compression stockings, and 48 per cent compared with mini-dose heparin. IPC devices significantly decreased the relative risk of DVT compared with placebo in high-risk patients such as neurosurgery and major orthopedic surgery patients and in modest risk patients such as general surgery patients. In major orthopedic surgery patients, the incidence of DVT was similar for IPC- and warfarin-treated patients; however, IPC was significantly better than warfarin at decreasing the incidence of calf only DVT, whereas warfarin seemed to be better at decreasing proximal DVT."22 More clinical studies are below.
What pressure does DVT therapy use?
"Foot compression, however, needs significantly higher pressures than calf compression, typically 130 mm Hg or more, compared with 40 mm Hg in the calf, there being a small amount of blood in the plantar venous plexus: about 20-30 mL, compared with 100-150 mL in the calf.23

Footnotes
- 1 Co, Annalisz. Intraoperative Measures for DVT Prophylaxis. Podiatry Institute. 4:2003. Page 18. (Last Accessed April-8-2020)
- 2 Turnbull, Betty. "Prevention of DVT after orthopaedic surgery: the AV Impulse System." British journal of Nursing 16.10 (2007): 612-615. (Last Accessed April-8-2020)
- 3 "DVT Prevention: Intermittent Pneumatic Compression Devices." Health Encyclopedia. University of Rochester Medical Center. Rochester, New York. (Last Accessed April-10-2020)
- 4 Siegal, Deborah, and Wendy Lim. "Venous thromboembolism." Hematology. Elsevier, 2018. 2102-2112. (Last Accessed April-10-2020)
- 5 Petrigliano, Frank A., and Jay R. Lieberman. "Venous Thromboembolic Disease after Total Hip Arthroplasty." Surgical Treatment of Hip Arthritis. WB Saunders, 2009. 390-398. (Last Accessed April-8-2020)
- 6 "Protect Yourself from Deep Vein Thrombosis with Sequential Compression Device (SCD)." University of Michigan Health System. UMHS Nursing Units. University of Michigan. 2013. Page 2. (Last Accessed April-13-2020)
- 7 "Graduated compression stockings" National Library of Medicine (Last Accessed April-13-2020)
- 8 Morris, Rhys J., and John P. Woodcock. "Evidence-based compression: prevention of stasis and deep vein thrombosis." Annals of surgery 239.2 (2004) Page 162. (Last Accessed April-2-2020)
- 9 Badireddy, Madhu, and Vasudeva Ranjit Mudipalli. "Deep Venous Thrombosis (DVT) Prophylaxis." (2018). (Last Accessed April-7-2020)
- 10 Badireddy, 2018. (Last Accessed April-7-2020)
- 11 Badireddy, 2018. (Last Accessed April-7-2020)
- 12 Badireddy, 2018. (Last Accessed April-7-2020)
- 13 Badireddy, 2018. (Last Accessed April-7-2020)
- 14 Fort, Charles W. "Get pumped up to prevent DVT." Nursing 2019. 32.9 (2002): 50-52. (Last Accessed April-10-2020
- 15 Maynard, Greg. "Preventing Hospital-Associated Venous Thromboembolism: A Guide for Effective Quality Improvement." Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. AHRQ Publication No. 16-0001-EF. August 2016. Page vii. (Last Accessed April-13-2020)
- 16 "Data and statistics on venous thromboembolism." Centers for Disease Control and Prevention. (2019). (Last Accessed April-7-2020)
- 17 Muhe E. Intermittent sequential high-pressure compression of the leg: a new method of preventing deep vein thrombosis. Am J Surg 1984; 147:781-5. (Last Accessed April-7-2020)
- 18 Bright, Linda Dove, and Sharon Georgi. "How to protect your patient from DVT." The American journal of nursing 94.12 (1994): 28-32. (Last Accessed April-13-2020)
- 19 Santori, F. S., et al. "Prophylaxis against deep-vein thrombosis in total hip replacement. Comparison of heparin and foot impulse pump." The Journal of bone and joint surgery. British volume 76.4 (1994): Pages 581-582. (Last Accessed April-13-2020)
- 20 Hull RD, Raskob GE, Gent M, et al. Effectiveness of intermittent pneumatic leg compression for preventing deep vein thrombosis after total hip replacement. JAMA 1990;263:2313-7. (Last Accessed April-2-2020)
- 21 Hills NH, Pflug JJ, Jeyasingh K, et al. Prevention of deep vein thrombosis by intermittent pneumatic compression of calf. BMJ 1972;1:131-5. (Last Accessed April-2-2020)
- 22 Vanek VW. Meta-analysis of effectiveness of intermittent pneumatic compression devices with a comparison of thigh-high to knee-high sleeves. Am Surg 1998;64(11):1050-8. (Last Accessed April-2-2020)
- 23 Morris and Woodcock. Page 165. (Last Accessed April-2-2020)

Medical Studies
-
 World Thrombosis Day. International Society on Thrombosis and Haemostasis. (Last Accessed April-2-2020)
World Thrombosis Day. International Society on Thrombosis and Haemostasis. (Last Accessed April-2-2020) -
 Maynard, Greg. "Preventing Hospital-Associated VenousThromboembolism: A Guide for Effective Quality Improvement." Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. AHRQ Publication No. 16-0001-EF. August, 2016. (Last Accessed April-2-2020)
Maynard, Greg. "Preventing Hospital-Associated VenousThromboembolism: A Guide for Effective Quality Improvement." Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. AHRQ Publication No. 16-0001-EF. August, 2016. (Last Accessed April-2-2020) -
 Gutt, Carsten N., et al. "Prophylaxis and treatment of deep vein thrombosis in general surgery." The American Journal of Surgery 189.1 (2005): 14-22. (Last Accessed April-2-2020)
Gutt, Carsten N., et al. "Prophylaxis and treatment of deep vein thrombosis in general surgery." The American Journal of Surgery 189.1 (2005): 14-22. (Last Accessed April-2-2020) -
 Fujiwara, Akira, Kosuke Ogata, and Michiya Hara. "The Use of Venous Foot Pump after Total Knee Arthroplasty An Experimental Study." Orthopedics & Traumatology 47.1 (1998): 370-373. (Last Accessed April-2-2020)
Fujiwara, Akira, Kosuke Ogata, and Michiya Hara. "The Use of Venous Foot Pump after Total Knee Arthroplasty An Experimental Study." Orthopedics & Traumatology 47.1 (1998): 370-373. (Last Accessed April-2-2020)
 Kwong, Louis M., and Andrew Luu. "DVT prophylaxis strategies following total joint arthroplasty." Seminars in Arthroplasty. Vol. 27. No. 1. WB Saunders, 2016. (Last Accessed April-2-2020)
Kwong, Louis M., and Andrew Luu. "DVT prophylaxis strategies following total joint arthroplasty." Seminars in Arthroplasty. Vol. 27. No. 1. WB Saunders, 2016. (Last Accessed April-2-2020) Fujisawa, Motoyuki, et al. "Effect of calf-thigh intermittent pneumatic compression device after total hip arthroplasty: comparative analysis with plantar compression on the effectiveness of reducing thrombogenesis and leg swelling." Journal of orthopaedic science 8.6 (2003): 807-811. (Last Accessed April-2-2020)
Fujisawa, Motoyuki, et al. "Effect of calf-thigh intermittent pneumatic compression device after total hip arthroplasty: comparative analysis with plantar compression on the effectiveness of reducing thrombogenesis and leg swelling." Journal of orthopaedic science 8.6 (2003): 807-811. (Last Accessed April-2-2020) Pitto, Rocco P., and Simon Young. "Foot pumps without graduated compression stockings for prevention of deep-vein thrombosis in total joint replacement: efficacy, safety and patient compliance." International orthopaedics 32.3 (2008): 331. (Last Accessed April-2-2020)
Pitto, Rocco P., and Simon Young. "Foot pumps without graduated compression stockings for prevention of deep-vein thrombosis in total joint replacement: efficacy, safety and patient compliance." International orthopaedics 32.3 (2008): 331. (Last Accessed April-2-2020) Giddings, J. C., et al. "Systemic haemostasis after intermittent pneumatic compression. Clues for the investigation of DVT prophylaxis and travellers thrombosis." Clinical & Laboratory Haematology 26.4 (2004): 269-273. (Last Accessed April-2-2020)
Giddings, J. C., et al. "Systemic haemostasis after intermittent pneumatic compression. Clues for the investigation of DVT prophylaxis and travellers thrombosis." Clinical & Laboratory Haematology 26.4 (2004): 269-273. (Last Accessed April-2-2020)
 Fordyce, M. J., and R. S. Ling. "A venous foot pump reduces thrombosis after total hip replacement." The Journal of bone and joint surgery. British volume 74.1 (1992): 45-49. (Last Accessed April-2-2020)
Fordyce, M. J., and R. S. Ling. "A venous foot pump reduces thrombosis after total hip replacement." The Journal of bone and joint surgery. British volume 74.1 (1992): 45-49. (Last Accessed April-2-2020) Anglen, J. O., et al. "Foot pump prophylaxis for deep venous thrombosis: the rate of effective usage in trauma patients." American journal of orthopedics (Belle Mead, NJ) 27.8 (1998): 580-582. (Last Accessed April-2-2020)
Anglen, J. O., et al. "Foot pump prophylaxis for deep venous thrombosis: the rate of effective usage in trauma patients." American journal of orthopedics (Belle Mead, NJ) 27.8 (1998): 580-582. (Last Accessed April-2-2020) Hull RD, Raskob GE, Gent M, et al. Effectiveness of intermittent pneumatic leg compression for preventing deep vein thrombosis after total hip replacement. JAMA 1990;263:2313-7. (Last Accessed April-2-2020)
Hull RD, Raskob GE, Gent M, et al. Effectiveness of intermittent pneumatic leg compression for preventing deep vein thrombosis after total hip replacement. JAMA 1990;263:2313-7. (Last Accessed April-2-2020)Product Videos
Smart Pneumatic Compression Video (1:41 minutes)
Vaso-Force DVT Prophylaxis Video (5:45 minutes)
Kendall SCD™ Sequential Compression Pump Video (1:41 minutes)
Logix PulStar Video (7:58 minutes)











Login and Registration Form