Online shopping provides a quick and convenient way to purchase products, and this is especially true for the...
Finger Pulse Oximeters - Adult, Pediatric
Finger Pulse Oximeters go by several different names, including finger oxygen reader, fingertip oximeter, or finger oxygen sensor. These medical devices are noninvasive clamp-on instruments that attach to a person's finger for diagnostics. Instead of the finger, attaching the clamp to a toe or an earlobe or toe is also suitable for accurate readings. These diagnostic devices measure two cardiac functions simultaneously—heart pulse and blood oxy
As mentioned above, these finger heart rate monitor combine two instruments to measure diagnostic signals from the circulatory system. They measure heart rate for bradycardia and tachycardia. They also measure SpO2 to detect blood oxygen saturation levels for hypoxemia.
Pulse Monitors
Pulse or heart rate measures beats per minute (bpm) of the heart muscle. An average resting heart rate ranges from 60 to 100 bpm. A tachycardia condition occurs when the heart rate is too fast or over 100 bpm while resting. A bradycardic situation takes place when the pulse is too slow. Athletes use heart rate monitors to help them achieve and maintain a target pulse rate while training. Target heart rates, based on individual age, get lower as people age. The chart below from the American Heart Association displays the target heart rates for safe exercise.
Age |
Target HR Zone |
Average Maximum Heart Rate |
|---|---|---|
20 years |
100-170 bpm |
200 bpm |
30 years |
95-162 bpm |
190 bpm |
35 years |
93-157 bpm |
185 bpm |
40 years |
90-153 bpm |
180 bpm |
45 years |
88-149 bpm |
175 bpm |
50 years |
85-145 bpm |
170 bpm |
55 years |
83-140 bpm |
165 bpm |
60 years |
80-136 bpm |
160 bpm |
65 years |
78-132 bpm |
155 bpm |
70 years |
75-128 bpm |
150 bpm |
The chart above displays the heart rate target zone by age. The far-right column depicts the average maximum heart rate for someone while conducting vigorous exercise. The figures are averages and serve only as a best practices guide for healthy exercise.1
"Heart rate is the most common parameter to determine the target exercise training intensity. The usual recommendations are in a range between 64% and 70% to 94% of HRmax…." The benefits of exercise intensity to the recommended target intensity follows "a dose-response relationship." The higher the dose within the constraints of the recommendations, the better the health results.2
Maintaining a targeted heart rate during exercise is crucial for health. Medical studies "confirm that there is irrefutable evidence of the effectiveness of regular physical activity in the primary and secondary prevention of several chronic diseases (e.g., cardiovascular disease, diabetes, cancer, hypertension, obesity, depression, and osteoporosis) and premature death…. There appears to be a linear relationship between physical activity and health. The connection increases with physical activity, and fitness will lead to additional improvements in health status.3
Finger pulse rate monitors are not just for use in targeting exercise intensity. These instruments are essential to determine healthy heart function. The health improvements from physical activity come from maintaining minimum training intensity, as referenced in the chart above. However, the recommended intensity "for patients with heart disease is generally 45% of heart rate reserve" which is slightly less than the lowest range in the center column of the chart. "Routine physical activity, whether as part of a job or as a leisure activity, is associated with reductions in the incidence of specific cancers, in particular colon and breast cancer. A systematic review of epidemiologic studies revealed that moderate physical activity (> 4.5 METs [equivalent to mowing the lawn]) was associated with a greater protective effect than activities of less intensity. Physically active men and women exhibited a 30%-40% reduction in the relative risk of colon cancer, and physically active women a 20%-30% reduction in the relative risk of breast cancer compared with their inactive counterparts."4
Product Profile

SpO2 Monitors
The second measurement these devices provide is the blood oxygen level (SaO 2, SPO2, or O2SAT). The device emits light waves that pass painlessly through the finger to a photodetector. The light wavelength measurement from its journey through the tissue and blood vessels provides an assessment of blood oxygenation. Finger oxygen sensors find use in-hospital diagnostics, operating rooms, medical clinics, and in-home care for at-risk patients. Below are links to more information.
These monitors detect the hemoglobin oxygen saturation in arterial blood, known as SPO2. Pulse oximetry can detect hypoxemia and related events.5 Pulse oximetry has established its position as the most convenient noninvasive method of monitoring arterial saturation continuously. Widely used in operating theatres and intensive care units, it is now being increasingly used in postoperative recovery units, on general wards, in the community, and during the transport of patients.6
Finger pulse oximetry has made a significant contribution to noninvasive monitoring in a wide variety of clinical situations. It allows for continuous reliable measurements of oxygen saturation while avoiding the discomfort and risks of arterial puncture. As the extent of hypoxic episodes during various procedures and clinical settings is better appreciated, the role of continuous noninvasive monitoring will undoubtedly expand.7
Using a finger pulse SPO2 can detect under-oxygenation in a patient before it reaches a dangerous level. While pulse oximeters monitor conscious patients, it's also common to use these devices while a patient is under the effects of anesthesia during surgery. SaO2 instruments help with sleep studies. They monitor to prevent sudden infant death syndrome (SIDS). They assist exercise and sports training to help athletes achieve and maintain a heart rate target zone, and they assist oxygen patients receiving adjunct oxygen therapy.
Sleep studies use pulse oximeters to monitor a patient's tendency to stop breathing during sleep. Sleep apnea creates low oxygen levels in the blood and interferes with the regular sleep cycle. These patients often complain of a lack of feeling well-rested. Some SaO2 devices have software that records the trend of oxygen saturation during a sleep cycle. Some of these devices come with alarms to signal when the saturation reaches a pre-set threshold.
Pulse oximetry is a well-established tool routinely used in many settings of modern medicine to determine a patient's arterial oxygen saturation and heart rate. The decreasing size of pulse oximeters over recent years has broadened their spectrum of use. For diagnosis and treatment of sleep-disordered breathing, overnight pulse oximetry helps determine the severity of disease and is used as an economical means to detect sleep apnea.8
Pulse oximetry is a safe, feasible test that adds value to existing screening. It identifies cases of critical congenital heart defects that go undetected with antenatal ultrasonography. The early detection of other diseases is an additional advantage.9
Types of O2SAT Devices
There are two types of fingertip attachable pulse oximeters—medical devices and non-medical devices. Medical devices meet the guidelines set by the FDA. Although non-medical devices fall short of the FDA guidelines, they still provide valuable diagnostics and give warning when someone should seek medical care.
FDA Approval
Finger oxygen monitors have approval by the FDA as "medical devices" requiring a prescription. However, many O2 Finger Sensors are sold in drugstores or over the Internet as over-the-counter products for non-medical purposes. A study examining non-medical O2 monitors found "no meaningful differences" between non-medical versions and the medically approved devices for measuring oxygen saturations between 90 to 99%. The non-medical devices work well to confirm normoxia or to rule out hypoxemia. However, patients testing below 90% should upgrade to using a medically approved device for improved accuracy.10, "FDA standards require a root mean square error (Arms) <3% over a saturation range of 70-100%."11
How an O2 Finger Sensor Works
Pulse oximetry uses the different light-absorbing characteristics of hemoglobin and oxyhemoglobin. The difference in the light absorption calculates the percentage of hemoglobin saturated with oxygen. An oximeter consists of a light emitter of red and infrared light and a sensor to collect the lightwaves after they pass through tissue. The probe attaches to a fingertip, toe, ear lobe, or an infant's heel. The sensor, positioned opposite the light emitter, detects the amount of light that passes through the capillaries. Oxyhemoglobin absorbs infrared light, and hemoglobin absorbs red light, allowing infrared light to pass through. A small computer module uses the data to calculate the level of blood oxygen saturation or SpO2.12
Advantages
- Noninvasive detection
- Easy to use
- Quick assessments
- Continuous monitoring available
- Alarm system available
- Monitors during exercise
- Monitors during sleep
- Monitors during medical procedures
Selecting the Best Fingertip Pulse Oximeter FOR SALE
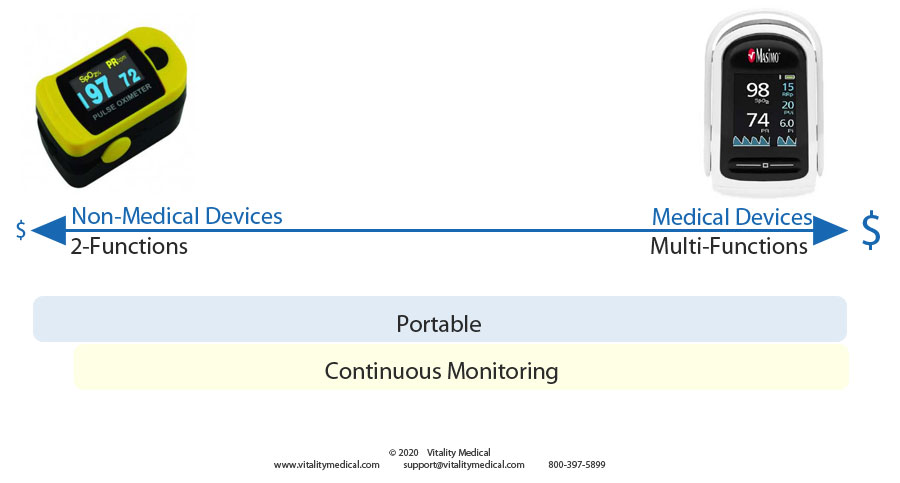
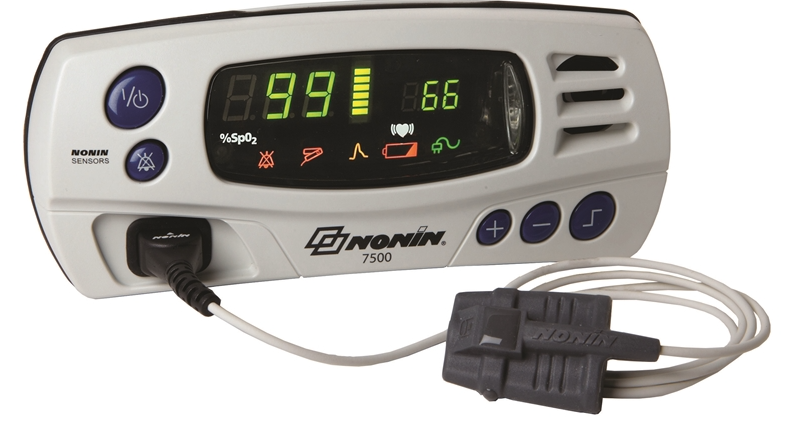
The pulse oximeter continuum above displays the two types of fingertip pulse oximeters with the medical-grade to the right and the non-medical devices to the left. Medical grade devices are more expensive than non-medical types. Two-function devices are the easiest to find and the least costly. Very few manufacturers make multi-functional devices. All of the finger oximeters are portable, and most offer continuous monitoring while only a very few offer just spot-checking capabilities.
Multi-functional oximeter devices may display additional numbers that measure other essential factors, such as Pi, RRpTM, and PVi. Pi indicates the Perfusion Index that shows blood circulation strength. RRpTM displays the number of breaths per minute. This indicator helps to determine heart and lung functioning. PVi is the Pleth Variation Index, which monitors changes in hydration, breathing effort, and perfusion. The Masimo Mightysat is an excellent example of a multi-functioning device. It is medical-grade quality and offers five separate tests, as shown in the image below.
Masimo Multi-Function Oximeter

Product Indications
- Pneumonia
- Cardiac disease
- Sepsis
- History of hypoxemia
- Sleep disorders
- Cardiac arrest
- Respiratory illness
- Lung cancer
- Asthma
- Anemia
- COPD
- Heart failure
Where to Use
- Surgery during anesthesia and postanesthesia
- Intensive care units (ICU)
- Hospitals
- Neonatal care units
- Neonatal intensive care units (NICU)
- Ambulance transportation
- Transport between hospital rooms
- Nursing homes
- Rehab
- Diagnostic testing
- Home care
How to Use
- Place one finger into the pulse oximeter clamp. Ensure the finger reaches the end of the device.
- Turn the oximeter on by pressing the ON/OFF button one
- For accurate results, keep hands still while taking a reading.
- The LED panel will light up with two numeric readings, one for pulse rate and the other for the blood saturation level.
- The pulse rate at rest should range between 60 and 100. Consult a physician if the reading does not fall within this range.
- SpO2 or blood saturation should read at 95% or above. Consult a physician if the reading is below this number.
- Fingernail polish or acrylic nails may produce inaccurate readings. In this case, turn your finger 90 degrees to allow light to shine through the sides of the finger, avoiding the fingernail.
Vitality Medical carries many different types of Pulse Oximeters supplies, including the following:
FAQ's
What does a fingertip pulse oximeter measure?
These pulse oximeter devices measure two critical cardiac-respiratory functions. The first is heart rate or the number of heartbeats per minute. This measurement allows an individual or clinician to monitor cardiac function. The second is the oxygenation level of the blood expressed as a percentage. This test checks how well the circulatory system is pumping oxygen throughout the body.
What are the best fingertip pulse oximeters?


Masimo MightySAT Oximeter
The Masimo MightySAT offers the best fingertip model available. It provides multiple functions with impressive accuracy. This device employs hospital-grade technology to measure during movement or low blood flow. It offers the added benefit of compatibility with smartphones. Display, track, trend, and share data with a compatible iOS or Android device on a free app.
How to read an SPO 2 device?
Two numbers post on the LED screen. The pulse rate tells how fast the heart is pumping blood throughout the body. At rest, the heart pumps slower. While exercising, the pulse rate pumps much quicker to keep up with the body's nutrient and oxygen needs. The oxygen saturation percentage is the other number that posts on the screen and should display within a 95-100% range. A number below 95% calls for caution and a phone call to a medical professional. A number below 90% indicates a trip to the emergency room for immediate medical attention.
How accurate are pulse oximeter devices?
During heart rate and SPO2 measurements, hands should be very still. Movement can contribute to inaccurate readings. Additionally, cold hands or poor blood circulation can also provide inaccurate readings. If you are cold, warm up and retest. The typical margin of error for one of these devices is 2%.
Can a pulse oximeter detect COVID-19?
Low oxygen levels in the blood are one of the signs of COVID-19. However, many patients can have COVID-19 without exhibiting low oxygen levels, so it is not the best testing device. A patient diagnosed with COVID-19 and self-quarantined at home may want to use a SpO2 instrument to monitor their oxygen saturation level to ensure it does not fall below 90%. When it goes below 90%, the patient should report to the hospital for additional treatments.
Product Videos
Respire Pulse Oximeter Video (1:05 minutes)
Using a Pulse Oximeter Video (2:43 minutes)
Demonstration Video (2:20 minutes)
Footnotes
- 1 Target Heart Rate Chart. American Heart Association. January 2015. (Last Accessed October-23-2020)
- 2 Hofmann, Peter, and Gerhard Tschakert. "Special needs to prescribe exercise intensity for scientific studies." Cardiology research and practice 2011 (2011). (Last Accessed October-23-2020)
- 3 Warburton, Darren ER, Crystal Whitney Nicol, and Shannon SD Bredin. "Health benefits of physical activity: the evidence." Cmaj 174.6 (2006): Page 801. (Last Accessed October-23-2020)
- 4 Warburton, Pages 802-803. (Last Accessed October-23-2020)
- 5 Pedersen, Tom, et al. "Pulse oximetry for perioperative monitoring." Cochrane Database of Systematic Reviews 3 (2014). (Last Accessed October-23-2020)
- 6 Hutton, Peter, and Tom Clutton-Brock. "The benefits and pitfalls of pulse oximetry." BMJ: British Medical Journal 307.6902 (1993): Page 457. (Last Accessed October-23-2020)
- 7 Schnapp, Lynn M., and Neal H. Cohen. "Pulse oximetry: uses and abuses." Chest 98.5 (1990): 1244-1250. (Last Accessed October-23-2020)
- 8 Netzer, Nikolaus, et al. "Overnight pulse oximetry for sleep-disordered breathing in adults: a review." Chest 120.2 (2001): 625-633. (Last Accessed October-23-2020)
- 9 Ewer, Andrew K., et al. "Pulse oximetry screening for congenital heart defects in newborn infants (PulseOx): a test accuracy study." The Lancet 378.9793 (2011): 785-794. (Last Accessed October-23-2020)
- 10 Hudson, Arlene J., et al. "Clinical interpretation of peripheral pulse oximeters labeled "not for medical use"." The Annals of Family Medicine 16.6 (2018): 552-554. (Last Accessed October 21, 2020)
- 11 Pulse Oximeters - Premarket Notification Submissions [510(k)s]: Guidance for Industry and Food and Drug Administration Staff. Guidance Document. U.S. Food and Drug Administration. March 2013. (Last Accessed October 21, 2020)
- 12 Booker, Rachel. "Pulse oximetry." Nursing Standard 22.30 (2008): 39-42. (Last Accessed October-23-2020)
Medical Studies
-
 Polevaya, S. A., et al. "Event-related telemetry of heart rate for personalized remote monitoring of cognitive functions and stress under conditions of everyday activity." Современные технологии в медицине 11.1 (eng) (2019). (Last Accessed October-23-2020)
Polevaya, S. A., et al. "Event-related telemetry of heart rate for personalized remote monitoring of cognitive functions and stress under conditions of everyday activity." Современные технологии в медицине 11.1 (eng) (2019). (Last Accessed October-23-2020) -
 Singh, Anupam Kumar, et al. "Comparative evaluation of accuracy of pulse oximeters and factors affecting their performance in a tertiary intensive care unit." Journal of Clinical and Diagnostic Research: JCDR 11.6 (2017): OC05. (Last Accessed October-23-2020)
Singh, Anupam Kumar, et al. "Comparative evaluation of accuracy of pulse oximeters and factors affecting their performance in a tertiary intensive care unit." Journal of Clinical and Diagnostic Research: JCDR 11.6 (2017): OC05. (Last Accessed October-23-2020) -
 Dubowitz, G., et al. "Accuracy of the Lifebox pulse oximeter during hypoxia in healthy volunteers." Anaesthesia 68.12 (2013): 1220-1223. (Last Accessed October-23-2020)
Dubowitz, G., et al. "Accuracy of the Lifebox pulse oximeter during hypoxia in healthy volunteers." Anaesthesia 68.12 (2013): 1220-1223. (Last Accessed October-23-2020)





Login and Registration Form