Buyer Guide for Lymphedema Pumps
Publish Date: April 24, 2020
Updated: December 8, 2021
By Burt Cancaster
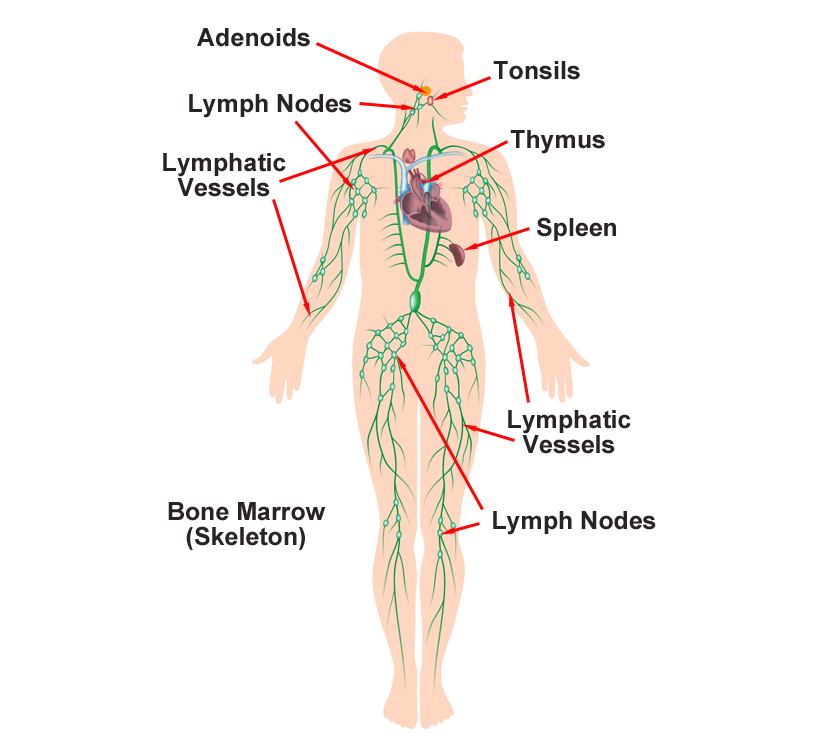
The Lymphatic System
The lymphatic system is part of the body’s immune system. It consists of a network of small vessels similar to the blood circulatory system through which lymph fluid journeys to tissues. It also includes valves, ducts, nodes, and organs. Lymph protects against infection and disease by removing bacteria and foreign material from tissues. This system also makes infection-fighting white blood cells. The lymphatic system includes the following organs of the human body:
- Spleen
- Thymus
- Lymph nodes
- Lymphatic vessels
- Tonsils
- Adenoids
- Bone marrow
The Lymphatic System
Lymphatic Disease
When the lymphatic system does not function properly, several disorders can arise. These disorders include Castleman’s disease, Hodgkin’s disease, lymphoma, lymphangitis, lymphocytosis, and lymphedema. Lymphedema occurs when lymph fails to circulate throughout the body. "The most readily recognizable attribute of lymphatic vascular incompetence is the presence of lymphedema, which arises as a consequence of insufficient lymph transport."1 "Lymphedema is a non-curative chronic swelling caused by impairment of the lymphatic system, affecting up to 250 million patients worldwide. The patients suffer from low quality of life because of discomfort and reduced range of motion due to the swelling."2
Surgical procedures and cancer treatment can precipitate lymphedema. When lymphedema exists, lymph fluid pools in the tissues causing swelling and pain. "Lymphedema is a set of pathologic conditions that are characterized by the regional accumulation of excessive amounts of interstitial protein-rich fluid. These occur as a result of an imbalance between the demand for lymphatic flow and the capacity of the lymphatic circulation."3
Blood vessels form a closed circulatory system, whereas lymphatic vessels form a one-way conduit for tissue fluid and leukocytes. In most vertebrates, the main function of lymphatic vessels is to collect excess protein-rich fluid that has extravasated from blood vessels and transport it back into the blood circulation. Lymphatic vessels have an important immune surveillance function, as they import various antigens and activated antigen-presenting cells into the lymph nodes and export immune effector cells and humoral response factors into the blood circulation. Defects in lymphatic function can lead to lymph accumulation in tissues, dampened immune responses, connective tissue and fat accumulation, and tissue swelling known as lymphedema.4
Lymphedema is a localized form of tissue swelling resulting from excessive retention of lymphatic fluid in the interstitial compartment and caused by impaired lymphatic drainage. Lymphedema is classified as primary or secondary. Primary lymphedema is caused by developmental lymphatic vascular anomalies. Secondary lymphedema is acquired and arises as a result of an underlying systemic disease, trauma, or surgery.
This progressive chronic disease has serious implications on patients’ quality of life. It is often misdiagnosed because it mimics other conditions of extremity swelling. There is no definitive cure for lymphedema. However, with proper diagnosis and management, its progression and potential complications may be limited.5
Patients with lymphedema have swelling and fibrosis of the affected region resulting in functional problems, decreased quality of life, and recurrent infections. In Western countries, secondary lymphedema is significantly more common and is most often due to lymphatic injury during the course of cancer treatment with risk factors such as extensive lymph node dissection and adjuvant chemoradiation therapy. These complications occur in various solid malignancies, including breast cancer, gynecological tumors, melanoma, and sarcoma. Because the incidence of lymphedema is directly correlated with survival time after oncologic therapy, it is likely that the number of patients who suffer from this disease will increase over time as life expectancy in cancer survivors is improved with better treatments. This is important since it is currently estimated that 5 million Americans are affected. Therefore, lymphedema is a great biomedical burden....6
Types of Lymphedema
There are two types of lymphedema. The first is primary lymphedema, which is rare. It affects 1 in 100,000 or .0001 percent. The other is secondary lymphedema, which affects 1 in 1,000 Americans.7 Primary lymphedema may result from Milroy’s disease, Meige’s disease, or late-onset lymphedema tarda. Again, these incidences are rare.
Any condition or surgical procedure that damages the lymph nodes or lymph vessels may cause secondary lymphedema. Removal of lymph nodes to prevent the spread of cancer or surgery that involves blood vessels in the arms or legs may help to generate this disease. Other causes include radiation treatment for cancer, cancer growth that blocks lymphatic vessels, an infection of the lymph nodes, or parasites that block lymph flow.
Secondary lymphedema often follows cancer treatment. The overall incidence of lymphedema following melanoma treatment is 16.35%. After genitourinary cancer treatments, it is 10.1%, and after gynecologic malignancies, it is 19.1%. The incidence of lymphedema is higher in the legs than in the upper extremities. "A recent meta-analysis reports the incidence of breast cancer–related lymphedema to range from 0 to 3% after lumpectomy alone to as high as 65% to 70% after modified radical mastectomy (removal of breast and axillary lymph nodes) with regional nodal radiation. Overall, 80% to 90% of women who will develop lymphedema do so within 3 years of treatment, but the risk persists years later as the remaining 10% to 20% will develop lymphedema at a rate of 1% per year. Petrek et al followed 263 patients and found that nearly 50% developed lymphedema by 20 years. These data suggest that lymphedema is probably more common than generally reported, and clearly the length of follow-up in a given study influences the reported incidence."8 "A prevalence of 20–27.2% has been reported for secondary lower-limb lymphedema (LLL) in patients who have undergone radical interventions, including pelvic lymph node dissection, radiation therapy, and/or chemotherapy, for gynecological cancer." 9
Lymphedema Observations

"Phlebolymphedema is a vascular condition that results in lower extremity edema from the combined effects of chronic venous insufficiency (CVI) and lymphedema. … Phlebolymphedema occurs in advanced forms of CVI as a pathophysiologic consequence of venous hypertension and related lymphatic overload. The condition can be aggravated by lymphatic damage from repeated episodes of cellulitis. There is a high incidence of venous leg ulcers (VLUs) among patients with phlebolymphedema driven by the severity of CVI in this population of patients and exacerbated by the edema."10
Lymphedema Risk Factors
There are three major contributing factors for developing this disease. The first is age. Older people are more susceptible to contracting this illness than younger. Second, is excessive weight. The more weight a person has, the higher the risk becomes for them. The last significant risk factor is the development of rheumatoid or psoriatic arthritis. These two forms of arthritis cause swelling within the lymph nodes, and thereby, impedes their functioning. Any of these three factors place people at risk. A combination of these factors constitutes a significant risk. Adding the variable of surgery or cancer puts people at the highest risk level for contracting lymphedema.
Lymphedema Prevention
The best prevention is not to get old. Unfortunately, we all age, so that is not a viable preventative measure. We can, however, watch our weight and exercise. Regular exercise is essential to good health. It helps to keep your weight in check and is the single most important thing you can do for your health. The second is your diet and weight. Eating the right foods and obtaining from foods that can harm you goes a long way to keeping your health and organ functions in the best working order. Our weight is also one of the most significant factors for our health. The more overweight you become, the more susceptible you become to a host of illnesses and diseases. Below is a chart that displays healthy weight versus risky weight for contracting lymphedema.
Lymphedema Risk by Weight
| BMI | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | 33 | 34 | 35 |
| Height (inches) | Body Weight (pounds) | ||||||||||||||||
| 58 | 91 | 96 | 100 | 105 | 110 | 115 | 119 | 124 | 129 | 134 | 138 | 143 | 148 | 153 | 158 | 162 | 167 |
| 59 | 94 | 99 | 104 | 109 | 114 | 119 | 124 | 128 | 133 | 138 | 143 | 148 | 153 | 158 | 163 | 168 | 173 |
| 60 | 97 | 102 | 107 | 112 | 118 | 123 | 128 | 133 | 138 | 143 | 148 | 153 | 158 | 163 | 168 | 174 | 179 |
| 61 | 100 | 106 | 111 | 116 | 122 | 127 | 132 | 137 | 143 | 148 | 153 | 158 | 164 | 169 | 174 | 180 | 185 |
| 62 | 104 | 109 | 115 | 120 | 126 | 131 | 136 | 142 | 147 | 153 | 158 | 164 | 169 | 175 | 180 | 186 | 191 |
| 63 | 107 | 113 | 118 | 124 | 130 | 135 | 141 | 146 | 152 | 158 | 163 | 169 | 175 | 180 | 186 | 191 | 197 |
| 64 | 110 | 116 | 122 | 128 | 134 | 140 | 145 | 151 | 157 | 163 | 169 | 174 | 180 | 186 | 192 | 197 | 2047 |
| 65 | 114 | 120 | 126 | 132 | 138 | 144 | 150 | 156 | 162 | 168 | 174 | 180 | 186 | 192 | 198 | 204 | 210 |
| 66 | 118 | 124 | 130 | 136 | 142 | 148 | 155 | 161 | 167 | 173 | 179 | 186 | 192 | 198 | 204 | 210 | 216 |
| 67 | 121 | 127 | 134 | 140 | 146 | 153 | 159 | 166 | 172 | 178 | 185 | 191 | 198 | 204 | 211 | 217 | 223 |
| 68 | 125 | 131 | 138 | 144 | 151 | 158 | 164 | 171 | 177 | 184 | 190 | 197 | 203 | 210 | 216 | 223 | 230 |
| 69 | 128 | 135 | 142 | 149 | 155 | 162 | 169 | 176 | 182 | 189 | 196 | 203 | 209 | 216 | 223 | 230 | 236 |
| 70 | 132 | 139 | 146 | 153 | 160 | 167 | 174 | 181 | 188 | 195 | 202 | 209 | 216 | 222 | 229 | 236 | 243 |
| 71 | 136 | 143 | 150 | 157 | 165 | 172 | 179 | 186 | 193 | 200 | 208 | 215 | 222 | 229 | 236 | 243 | 250 |
| 72 | 140 | 147 | 154 | 162 | 169 | 177 | 184 | 191 | 199 | 206 | 213 | 221 | 228 | 235 | 242 | 250 | 258 |
| 73 | 144 | 151 | 159 | 166 | 174 | 182 | 189 | 197 | 204 | 212 | 219 | 227 | 235 | 242 | 250 | 257 | 265 |
| 74 | 148 | 155 | 163 | 171 | 179 | 186 | 194 | 202 | 210 | 218 | 225 | 233 | 241 | 249 | 256 | 264 | 272 |
| 75 | 152 | 160 | 168 | 176 | 184 | 192 | 200 | 208 | 216 | 224 | 232 | 240 | 248 | 256 | 264 | 272 | 279 |
| 76 | 156 | 164 | 172 | 180 | 189 | 197 | 205 | 213 | 221 | 230 | 238 | 246 | 254 | 263 | 271 | 279 | 287 |
Chart Legend
| Normal | |
| Risky | |
| High Risk |
Lymphedema Treatment
Below is a list of the primary treatments for lymphedema diagnosed patients.
- Decongestive Lymphedema Therapy (DLT) mobilizes lymph and dissipates fibrosclerotic tissue
- Manual Lymph Drainage (MLD) lightly massages the affected area to increase lymph flow
- Pneumatic compression helps to drain tissues and is useful when infection is not likely
- Skincare is essential to prevent secondary infections
- Light exercise promotes lymph drainage and protein absorption
- Drug therapies offer pain control and treat seconday infections
- Surgery
- Vascularized Lymph Node Transfer (VLNT)
- Lymphaticovenous Anastomoses (LVA): VLNT and LVA are microsurgical procedures that can improve the patient's physiologic drainage of the lymphatic fluid and eliminate the need for compression garments in some patients. These procedures have better results when performed when a patient's lymphatic system has less damage.
- Suction-Assisted Protein Lipectomy (SAPL): Is more effective in later stages of lymphedema and allow removal of lymphatic solids and fatty deposits that are poor candidates for conservative lymphedema therapy, or VLNT or LVA surgeries.11
"Active exercise with compression therapy (AECT) is more effective than compression-only therapy (CT) for lower-limb lymphedema (LLL) that involves more marked pitting edema and/or harder skin. On the other hand, the immediate volume decrement from AECT is comparable to that from CT in LLL with less skin symptoms. … These results suggest that high-load AECT has marked effects on severe LLL."12 Relatively low pressures provide the better outcomes in the upper extremities, while pressures in the range of 40–60 mm Hg provide higher efficacy in the lower limbs. Scheduled therapy sessions overtime are alos necessary to achieve this efficacy. High pressures are unnecessary to treat chronic edema.13
In the United States pneumatic compression is the mainstay of lymphatic therapy. Intermittent pneumatic compression (IPC) preferably takes place with multi-chamber pumps, effectively removing fluid from the arms and legs. Adjunctive IPC therapy provides symptom relief and reduces episodes of cellulitis and ulceration in the legs. The use of certain IPCs shows significant reductions in cellulitis events, medical expenses, and the total cost of care. The benefits of IPC therapy for the promotion of lymph formation directly relate to the number of compressions applied and the time interval between each compression. Mechanical compression of the limb tissues promotes the formation of tissue conduits that provide functional outlets for the removal of edema fluid.14
"Compression modalities have been shown to be effective in reducing limb volume, increasing tissue elasticity and improving the physical, psychological, and aesthetic aspects of patient life. However, sustained volume reductions depend mostly on patient diligence."15
Advantages of Pneumatic Compression Therapy
- Easy operation
- Provides significant extravascular and lymphatic vascular movement
- provide significant edema reduction
- offers long-term maintenance
- can provide treatment equivalent in edema reduction outcome to in-clinic methods
- can maintain edema reduction after discharge from in-clinic sessions
- Reduces risk of cellulitis
- stimulates lymph uptake, propulsion, and movement, including transport of proteins in lymph fluid
- mimicks the lymphatic system, causing lymph fluid to move away from the limb towards the torso
- Decreases patient pain
- Decreases patient discomfort
- Improves patient quality of life
- Improves resource utilization
- Reduces treatment costs16
Disadvantages of Pneumatic Compression Therapy
- Offers patients self-management option
- Decreases the number of outpatient care visits
- Reduces need for rehabilitative treatments17
Anatomy of a Complete Compression System
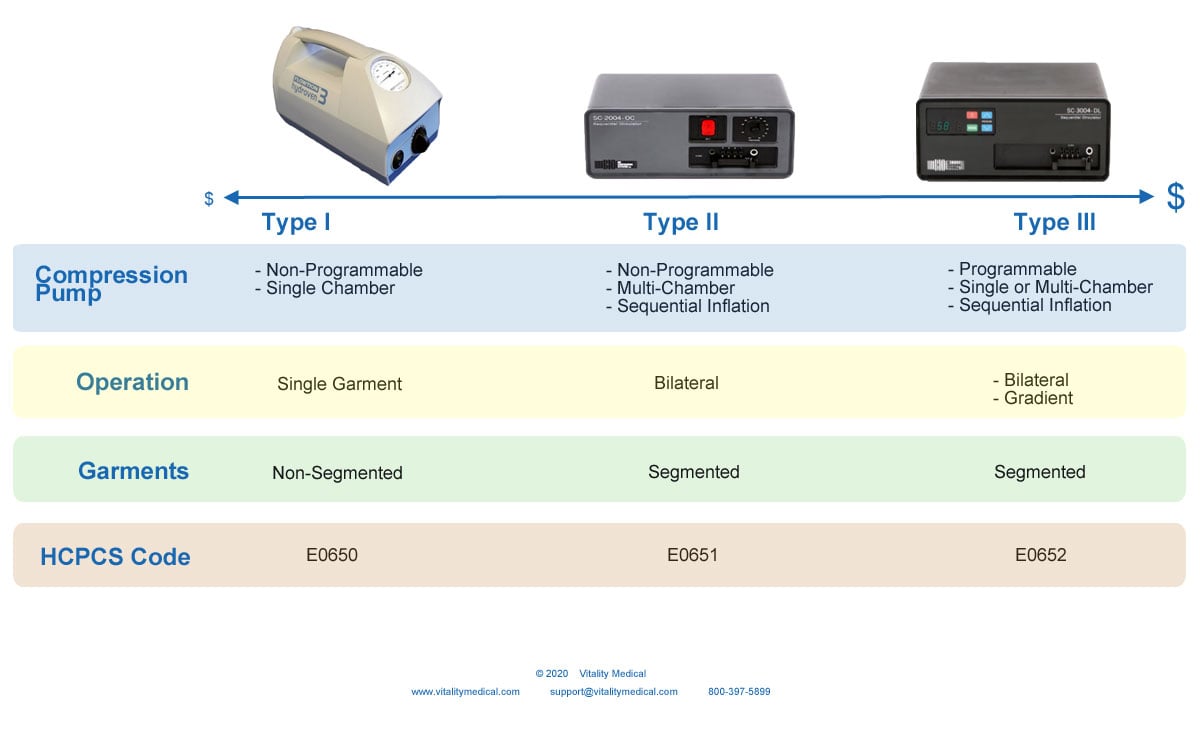
What Are the Types of Pneumatic Compression Pumps for Lymphedema?
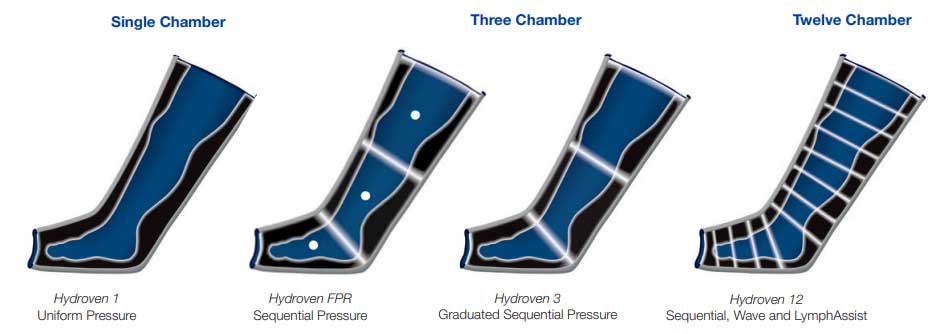
1. Pump, Non-programmable with Single Chamber and Non-segmented Garment
- Type I classification
- Single chamber pump (simplest design)
- Single outflow port
- Inflates and deflates on timed intervals
- Pre-set inflation and deflation
- Applies uniform pressure
- No manual control of pressure distribution
- No gradient pressure capability
- Adjustable pressure range: 1 to 100 mmHg
- Non-segmented, single bladder garment
- HCPCS Codes: E0650, E0655, E0660, E0665, E0666,
- Example: ArjoHuntleigh Hydroven 3
2. Pump, Non-programmable with Multi-chambers and Segmented Garment
- Type II classification
- Multi-chamber pump with 2 to 12 chamber capacity
- Multiple outflow ports
- Sequential inflation from distal to proximal
- Uniform deflation
- Fixed pressure for each chamber
- Adjustable pressure but limited programming options
- Bilateral operation: Treats up to two limbs simultaneously
- Segmented garment
- HCPCS Codes: E0651, E0656, E0657, E0667, E0668, E0669
- Example: Bio Compression SC2400
3. Pump, Programmable or Self-Calibrating with Single or Multi-chambers and Segmented Garment
- Type III classification
- Multi-chamber pump with 4 to 36 chambers
- Multiple outflow ports
- Multi-bladder garment
- Sequential inflation from distal to proximal
- Manually adjustable pressure levels
- Adjustable compression in each chamber (some models)
- Each chamber may have fixed or gradient pressure
- Provides at least 3-zones of pressure highest at the distal end and lowest at the proximal end
- Bilateral operation: Treats up to two limbs simultaneously
- Segmented garments
- HCPCS Codes: E0652, E0671, E0672, E0673
- Example: Bio Compression SC3400
Most pneumatic compression pumps today use intermittent compression cycles with inflation and deflation cycles either preset or programmable by the clinician. The sleeve or garment may have a single chamber design with one port or a multiple chamber design with one port per chamber. Pressure may be graded with the highest pressures in distal chamber segments. Depending on the specific manufacturer, compression cycles, treatment times, and compression levels may be either preset or programmable. Multi-chamber sequential compression pumps typically provide the greatest programming flexibility. Newer compression pump technology such as the Lympha-pants™ (LymphaCare, New York, NY) employs large multi-segment chambers that cover bilateral limbs and the lower or upper trunk simultaneously so that a comprehensive treatment may be delivered in a more efficient manner. The sequential inflation of chambers from distal to proximal in these devices is also thought to more naturally mimic lymph return.
"It is important to note that Type II compression pumps are set up to deliver either the same pressure in each chamber segment or a preselected pressure gradient in each chamber segment. However, specific chamber pressures cannot be programmed by the clinician. In comparison, type III compression pumps may be programmed by the clinician to deliver specific levels of compression over particular inflation and deflation cycles. Some type III pumps allow the clinician to program-specific levels of compression across each chamber segment."18
Lymphedema Compression Pump Selection Continuum
How to Select the Best Lymphedema Compression Pumps FOR SALE
There are three different types of Lymphedema Pumps and Sleeves to select. The first is a basic model that is non-programable, single-chambered, and provides pressure to a non-segmented garment. This device displays on the left of the continuum and is the model that Medicare favors and has the best chance of reimbursement approval. It is the least expensive option and works well for most lymphedema patients. An example of this type of lymphedema device is the ArjoHuntleigh Flowtron Hydroven 3
The next type is also non-programmable but offers multi-chambers, sequential inflation, and segmented garments. Sequential inflation allows compression therapy to begin at the distal end of the limb and climb up the limb towards the torso. This "milking" action forces lymph fluid out of the tissues and up the limb. Most of these devices are bilateral, allowing you to provide compression on more than one limb at a time. These devices display on the center of the continuum. An example of this type of lymphedema machine is the Bio Compression SC2400.
The third type of compression machine for lymphedema is programmable, single or multi-chambered, and offers sequential inflation. Many pumps of this type also offer gradient compression in which the pressure at the distal end is higher and gradually decreases toward the proximal end of the limb. This type uses segmented garments with multiple air pockets. They also offer bilateral functioning. They display on the far right of the continuum and are the most expensive devices used for treating lymphedema. Examples of this type of lymph compression device are the ArjoHuntleight Flowtron FPR and the Bio Compression SC3400
What is Continuous, Intermittent, Sequential, and Gradient Compression?
Continuous vs. Intermittent vs. Sequential vs. Gradient Compression
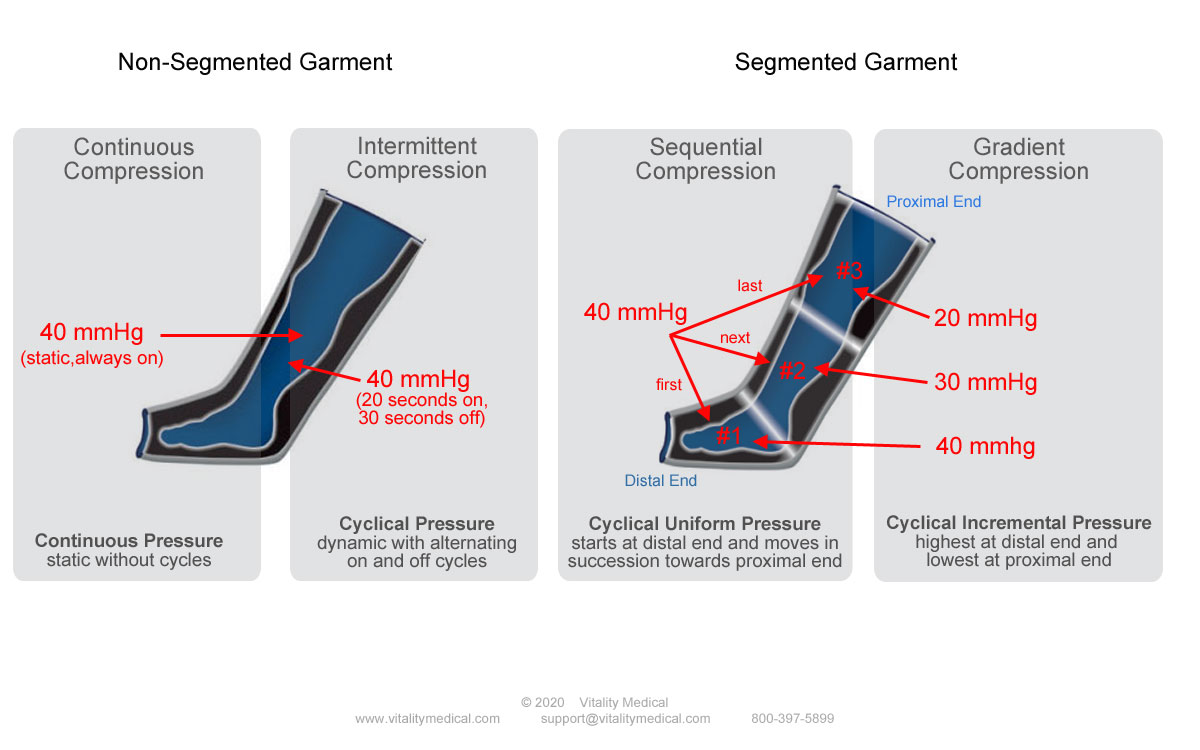
Continuous Compression
Continuous compression therapy most often takes place with a non-segmented or single segment garment. In the graphic above, the continuous modality displays on the far left column. Continuous therapy inflates single or multiple air bladders with the same amount of pressure in unison and sustains that pressure. That means if a multi-segmented garment is using continuous compression, all bladders fill with air simultaneously until the pressure reaches the set level. Medicare favors this static compression method since it is the least expensive and uses a simple, single-segmented garment in most instances.
Intermittent Compression
Cyclical pressure applied in an "ON" and then "OFF" again fashion is intermittent compression. Single or multiple sleeves fill with pressurized air and holds it for a set period and then deflates to release the pressure. The deflation period is then maintained for a set period and then the dynamic cycle begins again--inflating, holding, deflating, and then resting. The graphic above displays intermittent therapy in the second column. A typical intermittent therapy session would inflate to 40 mmHg, hold for 22 seconds, deflate and hold for 18 seconds. A therapy session like this might take place twice daily for one hour each dependent upon the needs of the patient.
Sequential Compression
The segmented leg garment pictured on the right of the graphic displays sequential compression in the third column. Sequential compression starts at the distal end of the leg to inflate the air bladder that is farthest from the torso. In the 3-chamber garment displayed, when chamber #1 fills with air to the pressure level of 40 mmHg, chamber #2 begins to fill. Once chamber #2 reaches 40 mmHg, chamber #3 begins to fill. The pressure is then held for a specified period and then deflates for a rest period. This succession process takes place repeatedly until the therapy is complete. The sequence of bottom to top pressure performs a "milking" action, forcing lymphatic fluid from the foot and leg tissues up the lymph vessels towards the torso.
Gradient Compression
Portrayed on the right side of the segmented garment in the fourth column of the graphic is gradient compression. This type of pressure also employs a multi-segmented garment. Gradient compression inflates the distal end of the garment with more pressure at the distal end than the proximal end. Each chamber moving up the leg fills with less pressure than the chamber below it. In the graphic, chamber #1, the farthest from the torso and the most distal, fills with 40 mmHg of pressure. Chamber #2 fills with less pressure to 30 mmHg. Chamber #3, the most proximal chamber fills to 20 mmHg, the least amount of pressure. This process forces lymph circulation up the leg towards the torso.
Sequential Gradient Compression
Also known as Sequential Graduated Compression, sequential gradient pressure mimics both types of compression displayed in columns three and four. The air bladders fill with air sequentially from the distal end towards the proximal. However, the chamber at the distal end fills with more pressure than the chambers above it. The combination of sequential and graduated compression reinforces the flow of fluids towards the body from the legs. In many cases, doctors prescribe lower pressures with this type of compression since the combination of sequential and gradient work together. This method offers the least amount of patient discomfort and is particularly useful for patients sensitive to pressure.
Lymphedema Indications
Below are some of the significant symptoms of lymphedema that may warrant the use of compression to prevent or treat lymphatic drainage issues.
- Inflammation
- Edema
- A feeling of fullness
- Puffiness
- A feeling of pressure
- Redness
- Pitting
- Deep aching sensation
- A feeling of heaviness
- Tightness
- Restricted range of motion
- Recurring infections
- Fibrosis (thickening or hardness of the skin)
- Hyperkeratosis
- Lymphangioma
- Lymphorrhea
If you notice any of these lymphedema symptoms, consult your doctor.
Lymphedema Pump Contraindications
There are few contraindications for the use of compression devices for lymphedema. The employment of compression pumps and sleeves to prevent or treat lymphedema symptoms should not take place if any of the following conditions exist with the patient.
- Edema due to congestive heart failure
- Serious arterial insufficiency
- Active phlebitis
- Deep vein thrombosis
- Localized wound infection
- Cellulitis19
- Local malignancy
- Undergoing anticoagulant therapy20
FAQ
- What causes lymphedema?
- What is the treatment for lymphedema?
- What is the life expectancy of someone with lymphedema?
- What foods should you eat to prevent or treat lymphedema?
- What foods should you avoid if you have lymphedema?
- Does drinking water help lymphedema?
- How do you massage lymphedema?
- What are the Medicare rules for lymphedema pump reimbursement?
- What pressure settings should lymphedema pump therapy use?
- How should I set the cycle times on the lymphedema pump for legs?
- How long should be the lymphedema pump treatment times?
- How often can I use a leg circulation pump?
- How effective is a compression pump therapy?
- How much does a lymphedema pump cost?
What causes lymphedema?
Secondary lymphedema develops when the lymph system no longer functions properly. Lymph fluid is not extracted from the tissues properly and conveyed up the lymph vessels to the torso. Fluid instead pools in the tissues of the limbs, causing swelling, pain, and other complications.
What is the treatment for lymphedema?
Management of lymphedema has historically focused on conservative measures, including physical therapy and the use of Lymphedema Compression Garments. More recently, surgery has been used for the treatment of secondary lymphedema.21 Most healthcare professionals prefer the least invasive measures first, starting with exercise, diet, compression stockings, and compression pumps.
"Unfortunately, there is no absolute cure for LE. On the other hand, effective treatment is available. Two main modalities include non-surgical and surgical options.... The mainstays of non-surgical lymphedema (LE) treatment modalities are complete decongestive therapy (CDT), compression therapy, advanced pneumatic compression pumps, and exercise. These treatments are effective mainly in early-stage LE.... Advanced Pneumatic Compression (APC) therapy can be used as an adjunct to CDT either in early or late phases. It mimics the pump effect of muscular contraction on the lymphatic system."22
"The primary treatment for lymphedema is a conservative approach known as complete decongestive therapy (CDT), which includes physical therapy, manual lymphatic drainage, and skincare. These treatments aim to decrease lymphatic fluid accumulation in the tissues by a variety of measures and are palliative in nature, aiming to prevent disease progression rather than cure the underlying pathology. Recent advances exploring pharmacotherapy and surgical treatments have shown some promise."23
What is the life expectancy of someone with lymphedema?
Treatment of mild cases of lymphedema with exercise and a healthy diet and compression stockings can restore normal fluid flows. However, chronic lymphedema requires additional treatments with pneumatic compression devices, drugs, or surgery. Most chronic lymphedema patients can receive regular treatments and mechanical support to increase lymphatic transport and maintenance. Through regular therapy and sometimes surgery, patients can expect a healthier life.
For years researchers and doctors considered lymphedema as "refractory or incurable." New advances are changing this perspective with a host of different therapies to use often in combinations to achieve positive outcomes.24
"Cancer-related lymphedema that develops into lymphangiosarcoma is serious. "The life expectancy of a patient with this condition is limited to a few months to 2 years."25
How do you unclog your lymphatic system?
Below is a list in order of priority of things you can do to improve the health of your lymphatic system.
- #1 Exercise daily for at least 30 minutes
- #2 Lose Weight
- #3 Wear compression stockings or sleeves
- #4 Use compression garments with compression pump
- #5 Hot and cold showers
- #6 Drink lots of water
- #7 Healthy diet
What foods should you eat to prevent or treat lymphedema?
The foods you eat play a significant role in your health. Below is a list of healthy foods you can eat that will contribute to a healthy lymph system.
- Fruits – cranberries, strawberries, peaches, blackberries, lemons, limes, oranges, grapefruit, honey dew melons, blueberries, avocados.
- Leafy green vegetables – kale, spinach, cabbage, watercress, romaine lettuce.
- Other vegetables – garlic, corn, squash, peppers, onions, mushrooms, herbs.
- Beans – black beans, butter beans, chickpeas, kidney beans, lentils, lima beans, peas, navy beans, pinto beans, great northern beans.
- Nuts – almonds, brazil, walnuts.
- Grains – flaxseed, chia, oats, millet, whole wheat, barley, brown rice, sorghum, quinoa, bulgur, teff, amaranth, buckwheat.

What foods should you avoid if you have lymphedema?
The following food items should be avoided by lymphedema patients.
- Processed foods
- Artificial sweeteners
- Meat products
- Dairy products
- Sugar
- Soy
- Salt
- Cheese
- Butter
Does drinking water help lymphedema?
Yes, drinking plenty of water supports proper lymph flow. Water can help manage the symptoms of lymphedema. It does not replace regular compression therapy.
How do you massage lymphedema?
For an arm massage, start at the tips of the fingers and gently do a sweeping motion with circumferential pressure towards your hand with enough pressure to move the surface of the skin. Continue up the hand towards the wrist, then up the wrist towards the elbow. Then continue past the elbow up towards the shoulder.
For a leg massage, begin at the toes and gently apply circumferential pressure sweeping up the toes towards the foot. Continue up the foot to the ankle and then up the ankle to the calf, and so on until you reach the upper thigh. Repeat the process starting from the toes.

What are the Medicare rules for leg compression machine for lymphedema reimbursement?
Medicare covers these pumps only after the patient undergoes a 4-week trial of conservative therapy. After the test, the patient’s physician must determine that conservative treatment is insufficient or that significant symptoms remain. The physician must further establish that the patient can tolerate a pneumatic pump, that an appropriate clinical response is achievable, and that the patient can adequately manage the device. Below are excerpts of the Medicare requirements.
Pneumatic compression pumps are only covered for purchase when the member has completed a successful trial. For the trial, the member must meet criteria: A (1 and 2) or B.
- A four (4) week trial rental will be covered for Primary and Secondary Lymphedema if:
1. The member has undergone a four (4)-week attempt of conservative therapy that must include the use of an appropriate compression bandage system or compression garment, exercise, and elevation of the limb;
And
2. The treating physician determines that there has been no significant improvement or significant symptoms remain after the conservative therapy;
OR
- A four (4) week trial rental will be covered for Venous Stasis Ulcers if:
1. The member has edema of the affected lower extremity, one or more venous stasis ulcer(s) which have failed to heal after a six (6)-month trial of conservative therapy including a compression bandage system or compression garment, appropriate dressings for the wound, exercise, and elevation of the limb.
- Once the trials are completed, purchase is covered if the additional criteria below are met:
- The four (4)-week rental trial of the pneumatic compression device was accomplished, and
- The patient can tolerate the device, and 3. In the provider’s opinion there has been an appropriate clinical response, and 4. The member can properly manage the device.
WHEN COVERAGE WILL NOT BE APPROVED
- For indications other than cited above.
- When the medical guidelines shown above are not met.
- Appliances used for pneumatic compression of the chest or trunk (E0656 and E0657) will be denied as not medically necessary.
- PCD E0675 used in the treatment of peripheral arterial disease is not reasonable and necessary and therefore not covered.
LIMITATIONS
The use of pneumatic compression devices is contraindicated in those individuals with active infection, metastatic disease, or radiation for lymphedema. Contraindications for CVI include serious arterial insufficiency, edema due to congestive heart failure, phlebitis, deep vein thrombosis, or a localized wound infection or cellulitis.
BILLING/ CODING/PHYSICIAN DOCUMENTATION INFORMATION
This policy may apply to the following codes. Inclusion of a code in this section does not guarantee reimbursement.
Applicable codes: E0650, E0651, E0652, E0655, E0656, E0657, E0660, E0665, E0666, E0667, E0668, E0669, E0670, E0671, E0672, E0673, A6545….
Non-segmented Compression Devices
When a pneumatic compression device is covered, a non-segmented device (E0650) or segmented device without manual control of the pressure in each chamber (E0651) is generally sufficient to meet the clinical needs of the patient.
- A non-segmented compressor (E0650) with a segmented appliance/sleeve (E0671- E0673) is considered functionally equivalent to an E0651 compressor with a segmented appliance/sleeve (E0667-E0669).
Segmented Compression Devices
When a segmented device with manual control of the pressure in each chamber (E0652) is ordered and provided, payment will be based on the allowance for the least costly medically appropriate alternative, E0651, unless there is clear documentation of medical necessity in the individual case. (Examples may be significant skill scars or the presence of contracture or pain caused by a clinical condition that requires more costly manual control.)
Full coverage for code E0652 will be approved only when there is documentation that the individual has unique characteristics that prevent satisfactory pneumatic compression treatment using a non-segmented device (E0650) with a segmented appliance/sleeve (E0671-E0673) or a segmented device without manual control of the pressure in each chamber (E0651).26
Medicare reimburses for leg pumps for edema under three different HCPCS codes: E0650, E065 1, and E0652. Generally, lymphedema pump arm machines are classified as either segmented or nonsegmented, depending on whether distinct segments of the devices can be inflated sequentially. The less sophisticated, and least expensive pumps, are coded E0650 and E065 1, and cost Medicare about $600 and $800, respectively. The most sophisticated and expensive pumps are coded E0652 and cost Medicare about $4,000 to $6000. This device is characterized by calibrated gradient pressure, capable of delivering individually determined pressure to each segmental unit.27
What pressure settings should lymphedema pump therapy use?
The level of pressure is dependent upon the individual needs of the patient. Your doctor should prescribe the correct therapy for your individual needs. Medical studies indicate the use of pneumatic compression machines with pressures "ranging between 35 and 180 mm-Hg, pump pressures are adjusted to mostly 20–60 mm-Hg [for actual treatment]. The pressure must be individualized in order to prevent skin damage during application. APC therapy was found beneficial in reducing LE, whereas compression sleeves prevented additional swelling without influencing volume reduction.28
"The pressure used must be sufficient to overcome the resistive forces within the tissue being treated, and in lymphatic obstruction, the subcutaneous tissue pressure can be significantly elevated with pressures in edematous lymphatics and tissues ranging from 15 to 18 mmHg. A peak inflation pressure of 25 to 50 mmHg might be sufficient for most patients in the absence of significant fibrosis…. A sustained pressure of 60-70 mmHg may be considered as the maximum upper limit." 29
One study found that treatment pressures should range from 20 to 90 mmHg depending upon the clinician's assessment.30
Other studies found "that patients complained of pain at pressures greater than 41-60 mmHg...." 31
An instructor for lymphedema certification states that "Because every patient’s lymphedema and response to treatment is unique, there is no universal pressure setting that works for all. Also, there are no established guidelines for the optimal pressure value. A recent systematic literature review published in the Journal of Lymphology (2012) revealed that 'A peak inflation pressure of 25-50 mmHg might be sufficient for most patients in the absence of significant fibrosis.' Personally, I recommend approx. 40 mmHg pressure for patients with upper extremity lymphedema and 50 mmHg for patients with lower extremity lymphedema, with an upper limit of 50 mmHg and 60 mmHg respectively."32
Treatment pressures are selectable according to clinician assessment from 20 to 90 mmHg."33
"Advanced Pneumatic Compression (APC) therapy can be used as an adjunct to CDT either in early or late phases. It mimics the pump effect of muscular contraction on the lymphatic system. Ranging between 35 and 180 mm-Hg, pump pressures are adjusted to mostly 20–60 mm-Hg (2, 12). The pressure must be individualized in order to prevent skin damage during application. APC therapy was found beneficial in reducing LE, whereas compression sleeves prevented additional swelling without influencing volume reduction."34
One study with breast cancer patients used the Lympha Press® with a pressure of 40-60 mmHg with success.35
In an application to the forearm pressure settings of between 9.0 ± 4.2 mmHg and 13.7 ± 4.8 mmHg produced successful results.36
Lymphatic vessels are known to collapse when pressure exceeds 30 mm Hg, obstructing the drainage, and for this reason the upper extremity is treated with 30 mm Hg pressure and for the lower extremity pressures range from 35 to 40 mm Hg.37
Lymphedema Compressor and Garments

How should I set the cycle times on the sequential compression device for edema?
One study found that cycle times of 50 seconds was optimal for patients in the test.38 An arm garment with 4 separate segments with each segment set to inflate sequentially at a rate of 18 seconds per chamber until all chambers are fully inflated for a total inflation time of approximately 72 seconds worked best in another test. Full garment inflation is then held for 22 seconds before all chambers simultaneously deflate for 18 seconds.39
How long should treatments be with a lymphedema pump?
Treatment durations should vary depending upon your needs and tolerance. Most doctors recommend at least 30 minutes daily but you may require more for your condition. Some people only need treatment for a few weeks and they are done. Consult with your doctor for your individual needs. Below are some excerpts from medical studies.
In an attempt to reduce edema of the arm after mastectomy, patients were provided with an elastic sleeve which was worn for a period of between 1 week and up to 6 months. A statistically significant mean relative decrease of 17% in the volume of edema was achieved. Subsequent treatment by intermittent pneumatic compression for 10 days produced a further significant mean relative decrease of 18%. When the sleeve was worn for 6 months after this treatment there was no significant increase in arm volume--that is, no relapse.40
One study recommended a treatment duration of 1 to 2 hours per day.41 Another found that a duration of ½ to 1-1/2 hours to be sufficient.42 An noted study indicates that a combination of manual lymphatic drainage for 45 minutes and pneumatic compression daily for two hours was best. This procedure took place for a period 2-weeks and significantly decreased patient arm volume following breast cancer treatment.43
In another study had patients wearing an elastic sleeve for 1 week to 6 months showing a 17% decrease in volume. Subsequent treatment by intermittent pneumatic compression for 10 days produced a further significant volume decrease of 18%.44
How often can I use a compression pump for legs?
Most doctors recommend daily use of the pump if you have chronic edema. Many patients with mild symptoms use the pump for 2-weeks or less. Some patients only use the pump following their surgery within the hospital for a few days. Follow your doctor's instructions.
How effective is a lymphedema pump leg device?
Modern studies demonstrate the positive outcomes of using a mechanical compression device. Doctors often employ these devices during the hospital visit immediately following a surgical procedure to reduce edema. Should swelling continue to be an issue or if there is a chronic problem, your doctor may prescribe home use of pneumatic compression. There are few negative side effects when use is in conformance with known indications and withheld for known contraindications.
How much does a lymphedema machine cost?
The cost of lymphedema compression pumps range between $400 to $6,500. The compression garments are usually sold separately based upon location (arm, leg, leg to foot, etc.) and size. Prices for garments range from $60 to $400.
What are segmented and non-segmented lymphedema garment sleeves?
A non-segmented garment has a single air bladder that fills with air from a compression device. A segmented or multi-segmented garment has more than one air bladder. The segmented garments offer enhanced treatment capabilities by providing for sequential inflation, gradual inflation, or a combination of sequential gradual compression and other types of lymphedema therapies.
Lymphedema Garment Options
Footnotes
- 1 Rockson, Stanley G. "Diagnosis and management of lymphatic vascular disease." Journal of the American College of Cardiology 52.10 (2008): 799-806. (Last Accessed April-16-2020)
- 2 Schaverien, Mark V., Julie A. Moeller, and Sarah D. Cleveland. "Nonoperative treatment of lymphedema." Seminars in plastic surgery. Vol. 32. No. 01. Thieme Medical Publishers, 2018. (Last Accessed April-16-2020)
- 3 Warren, Anne G., et al. "Lymphedema: a comprehensive review." Annals of plastic surgery 59.4 (2007): 464-472. (Last Accessed April-16-2020)
- 4 Alitalo, Kari. "The lymphatic vasculature in disease." Nature medicine 17.11 (2011): 1371. (Last Accessed April-16-2020)
- 5 Grada, Ayman A., and Tania J. Phillips. "Lymphedema: pathophysiology and clinical manifestations." Journal of the American Academy of Dermatology 77.6 (2017): 1009-1020. (Last Accessed April-17-2020)
- 6 Ly, C.L.; Kataru, R.P.; Mehrara, B.J. Inflammatory Manifestations of Lymphedema. Int. J. Mol. Sci. 2017, 18, 171. (Last Accessed April-20-2020)
- 7 Sleigh, Bryan C., and Biagio Manna. "Lymphedema." StatPearls [Internet]. StatPearls Publishing, 2019. (Last Accessed April-20-2020)
- 8 Mclaughlin, Sarah A. "Lymphedema: separating fact from fiction." Cancer 26.3 (2012). (Last Accessed April 20, 2020)
- 9 Fukushima, Takuya, et al. "Immediate effects of active exercise with compression therapy on lower-limb lymphedema." Supportive Care in Cancer 25.8 (2017): 2603-2610. (Last Accessed April 20, 2020)
- 10 Lerman, Michelle, et al. "Health and economic benefits of advanced pneumatic compression devices in patients with phlebolymphedema." Journal of vascular surgery 69.2 (2019): 571-580.
- 11 Sleigh, Bryan C., and Biagio Manna. "Lymphedema." StatPearls [Internet]. StatPearls Publishing, 2019. (Last Accessed April-20-2020)
- 12 Fukushima, 2019. (Last Accessed April-20-2020)
- 13 Mosti, Giovanni, and Attilio Cavezzi. "Compression therapy in lymphedema: Between past and recent scientific data." Phlebology 34.8 (2019): 515-522. (Last Accessed April-20-2020)
- 14 Rockson, Stanley G. "Intermittent pneumatic compression therapy." Lymphedema. Springer, Cham, 2018. 443-448. (Last Accessed April-20-2020)
- 15 Rosas, Francisca, Ivone Silva, and Rui de Almeida. "NON-SURGICAL TREATMENTS OF LYMPHEDEMA OF THE LOWER LIMBS." Angiologia e Cirurgia Vascular 15.2 (2019): 97-112. (Last Accessed April-20-2020)
- 16 Aldrich, Melissa B., et al. "Effect of pneumatic compression therapy on lymph movement in lymphedema-affected extremities, as assessed by near-infrared fluorescence lymphatic imaging." Journal of innovative optical health sciences 10.02 (2017): 1650049. (Last Accessed April-20-2020)
- 17 Hand, Larry. Lymphedema Patients Benefit from Pneumatic Compression Devices. The Hospitalist. (11) 2015. (Last Accessed April-22-2020)
- 18 Conner-Kerr, Teresa. Pneumatic Compression Pump Therapy: An Evidence-based Approach to the Treatment of Chronic Vascular Disorders. Today's Wound Clinic. 2:1 Winter 2008. (Last Accessed April-22-2020)
- 19 Decision Memo for PNEUMATIC Compression Pumps for Venous Insufficiency (CAG-00075N). Centers for Medicare & Medicaid Services. October 2001. (Last Accessed April-22-2020)
- 20 Schaverien, Mark V., Julie A. Moeller, and Sarah D. Cleveland. "Nonoperative treatment of lymphedema." Seminars in plastic surgery. Vol. 32. No. 01. Thieme Medical Publishers, 2018. (Last Accessed April-20-2020)
- 21 Chang, David W., et al. "Lymphedema: surgical and medical therapy." Plastic and reconstructive surgery 138.3S (2016): 209S-218S. (Last Accessed April-20-2020)
- 22 Kayıran, Oğuz, et al. "Lymphedema: From diagnosis to treatment." Turkish journal of surgery 33.2 (2017): 51. (Last Accessed April-20-2020)
- 23 Ly, C.L.; Kataru, R.P.; Mehrara, B.J. Inflammatory Manifestations of Lymphedema. Int. J. Mol. Sci. 2017, 18, 171. (Last Accessed April-20-2020)
- 24 Warren, Anne G., et al. "Lymphedema: a comprehensive review." Annals of plastic surgery 59.4 (2007): 464-472. (Last Accessed April-20-2020)
- 25 Mihara, Makoto, et al. "Pathological steps of cancer-related lymphedema: histological changes in the collecting lymphatic vessels after lymphadenectomy." PloS one 7.7 (2012). (Last Accessed April-20-2020)
- 26 Pneumatic Compression Device. Medicare Part C Medical Coverage Policy. BlueCross Blue Shield of North Carolina. March 2019. Pages 2-4. (Last Accessed April-20-2020)
- 27 Medicare Allowance for Lymphedema Pumps. Department of Health and Human Services. OEI-04-97-00130. July 1998. Page 1. (Last Accessed April-20-2020)
- 28 Kayıran, Oğuz, et al. "Lymphedema: From diagnosis to treatment." Turkish journal of surgery 33.2 (2017): 51. (Last Accessed April-20-2020)
- 29 Feldman, J. F., et al. "Intermittent pneumatic compression therapy: a systematic review." Lymphology 45.1 (2012): 13-25. Page 21. (Last Accessed April-20-2020)
- 30 Aldrich, (Last Accessed April-20-2020)
- 31 Karafa, M., A. Karafova, and A. Szuba. "The effect of different compression pressure in therapy of secondary upper extremity lymphedema in women after breast cancer surgery." Lymphology 51.1 2018. Page 35. (Last Accessed April-20-2020)
- 32 Klose, Guenter. "To Pump or Not to Pump..." Klose Training Lymphedema Certification. November, 2013. (Last Accessed April-20-2020)
- 33 Pilch, U., Wozniewski, M., Szuba, A. "Influence of Compression Cycle Time and Number of Sleeve Chambers on Upper Extremity Lymhedema Volume Reduction During Intermittent Pneumatic Compression." Lymphology 42 (2009) page 26-35. (Last Accessed April-20-2020)
- 34 Kayıran, Page 51. (Last Accessed April-20-2020)
- 35 Johansson K, Lie E, Ekdahl C, Lindfeldt J. A randomized study comparing manual lymph drainage with sequential pneumatic compression for treatment of postoperative arm lymphedema. Lymphology 1998; 31 (02) 56-64. (Last Accessed April-20-2020)
- 36 Fife CE, Davey S, Maus EA, Guilliod R, Mayrovitz HN. A randomized controlled trial comparing two types of pneumatic compression for breast cancer-related lymphedema treatment in the home. Support Care Cancer 2012; 20 (12) 3279-3286. (Last Accessed April-20-2020)
- 37 Schaverien, Mark V., Julie A. Moeller, and Sarah D. Cleveland. "Nonoperative treatment of lymphedema." Seminars in plastic surgery. Vol. 32. No. 01. Thieme Medical Publishers, 2018. (Last Accessed April-20-2020)
- 38 Aldrich, (Last Accessed April-20-2020)
- 39 Fife, (Last Accessed April-24-2020)
- 40 Swedborg I. Effects of treatment with an elastic sleeve and intermittent pneumatic compression in post-mastectomy patients with lymphoedema of the arm. Scand J Rehabil Med 1984; 16 (01) 35-41. (Last Accessed April-20-2020)
- 41 Schaverien, Mark V., Julie A. Moeller, and Sarah D. Cleveland. "Nonoperative treatment of lymphedema." Seminars in plastic surgery. Vol. 32. No. 01. Thieme Medical Publishers, 2018. (Last Accessed April-20-2020)
- 42 Aldrich, 2017 (Last Accessed April-20-2020)
- 43 Johansson K, Lie E, Ekdahl C, Lindfeldt J. A randomized study comparing manual lymph drainage with sequential pneumatic compression for treatment of postoperative arm lymphedema. Lymphology 1998; 31 (02) 56-64. (Last Accessed April-20-2020)
- 44 Swedborg I. Effects of treatment with an elastic sleeve and intermittent pneumatic compression in post-mastectomy patients with lymphoedema of the arm. Scand J Rehabil Med 1984; 16 (01) 35-41. (Last Accessed April-20-2020)
-
 Yoo, Hye Ju, et al. "Wearable Lymphedema Massaging Modules: Proof of Concept using Origami-inspired Soft Fabric Pneumatic Actuators." 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR). IEEE, 2019. (Last Accessed April-16-2020)
Yoo, Hye Ju, et al. "Wearable Lymphedema Massaging Modules: Proof of Concept using Origami-inspired Soft Fabric Pneumatic Actuators." 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR). IEEE, 2019. (Last Accessed April-16-2020) -
 Tunis, S. Whyte, J. Ballantine, L. Ulrich, M. Decision Memo for Lymphedema Pumps - CAG-00016N. Centers for Medicare & Medicaid Services. CMS.gov May 2001. (Last Accessed April-16-2020)
Tunis, S. Whyte, J. Ballantine, L. Ulrich, M. Decision Memo for Lymphedema Pumps - CAG-00016N. Centers for Medicare & Medicaid Services. CMS.gov May 2001. (Last Accessed April-16-2020) -
 Szolnoky G, Lakatos B, Keskeny T. , et al. Intermittent pneumatic compression acts synergistically with manual lymphatic drainage in complex decongestive physiotherapy for breast cancer treatment-related lymphedema. Lymphology 2009; 42 (04) 188-194. (Last Accessed April-16-2020)
Szolnoky G, Lakatos B, Keskeny T. , et al. Intermittent pneumatic compression acts synergistically with manual lymphatic drainage in complex decongestive physiotherapy for breast cancer treatment-related lymphedema. Lymphology 2009; 42 (04) 188-194. (Last Accessed April-16-2020) -
 Szuba A, Achalu R, Rockson SG. Decongestive lymphatic therapy for patients with breast carcinoma-associated lymphedema. A randomized, prospective study of a role for adjunctive intermittent pneumatic compression. Cancer 2002; 95 (11) 2260-2267. (Last Accessed April-16-2020)
Szuba A, Achalu R, Rockson SG. Decongestive lymphatic therapy for patients with breast carcinoma-associated lymphedema. A randomized, prospective study of a role for adjunctive intermittent pneumatic compression. Cancer 2002; 95 (11) 2260-2267. (Last Accessed April-16-2020) -
 Muluk SC, Hirsch AT, Taffe EC. Pneumatic compression device treatment of lower extremity lymphedema elicits improved limb volume and patient-reported outcomes. Eur J Vasc Endovasc Surg 2013; 46 (04) 480-487. (Last Accessed April-16-2020)
Muluk SC, Hirsch AT, Taffe EC. Pneumatic compression device treatment of lower extremity lymphedema elicits improved limb volume and patient-reported outcomes. Eur J Vasc Endovasc Surg 2013; 46 (04) 480-487. (Last Accessed April-16-2020) -
 Pappas CJ, O'Donnell Jr TF. Long-term results of compression treatment for lymphedema. J Vasc Surg 1992; 16 (04) 555-562 , discussion 562–564. (Last Accessed April-16-2020)
Pappas CJ, O'Donnell Jr TF. Long-term results of compression treatment for lymphedema. J Vasc Surg 1992; 16 (04) 555-562 , discussion 562–564. (Last Accessed April-16-2020)
Medical Studies
Product Videos
Lymphatic Disorder Treatments Review Video (1:12 minutes)
Lymphedema A to Z Video (8:12 minutes)

Burt Cancaster, Author
Vitality Medical
7910 South 3500 East, Suite C
Salt Lake City,
UT
84121
(801) 733-4449
[email protected]
Vitality Medical


Login and Registration Form